Relationship between habits and precancerous lesions of the oral cavity – a clinicopathological study
Abstract
Introduction: Oral cancers account for 3% of total malignancies. A research was conducted to find the incidence, age, and sex distribution, clinical presentation, and the relationship between habits and various premalignant lesions of the oral cavity.
Methods: It was a hospital-based observational and cross-sectional study, conducted in GSL Medical College, Rajamahendravaram from October 2015 to April 2017. Individuals aged > 18 years, with leukoplakia, erythroplakia, blanched mucosa with or without fibrous bands and /or trismus suggestive of oral submucous fibrosis, bilateral whitish lesions with a reticular pattern suggestive of lichen planus, and ulcer against sharp tooth denture suggestive of traumatic dental ulcers were taken. Individuals with frank oral malignancy, those with terminal diseases, those who did not submit informed consent were not considered.
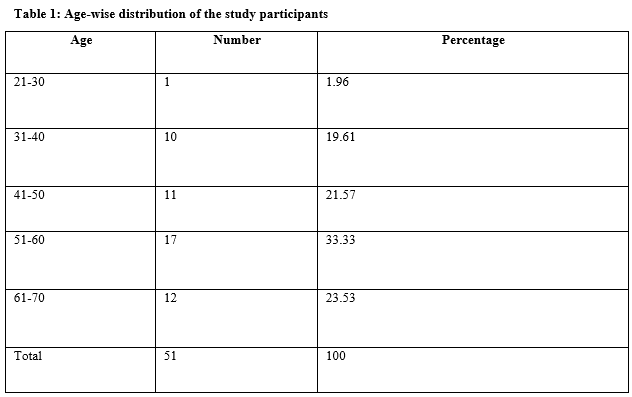
Results: The majority of patients (33.33%) were aged between 51 – 60 years, belong (62.75%) to lower socioeconomic status. Leukoplakia (64.7%) was a common clinical presentation. Most (49.02%) of the study patients presented with a burning sensation. When addictions were considered, 86.27% of patients were smokers, 23.53% were addicted to alcohol.
Conclusion: Leukoplakia was the commonest (64.71%) premalignant lesion, 51 – 60 years was the common age group. Premalignant lesions were most commonly seen among males, most of the study participants belong to low and middle socio-economic groups with a rural background. Diabetes mellitus was the most common comorbidity associated with premalignant lesions.
Downloads
References
Kademani D. Oral cancer. Mayo Clin Proc. 2007;82(7):878-887. doi: 10.4065/82.7.878.
Silverman S Jr. Demographics and occurrence of oral and pharyngeal cancers. The outcome, the trends, the challenge. J Am Dent Assoc. 2001;132:7S-11S. doi: 10.14219/jada.archive.2001.0382.
Ries LAG, Melbert D, Krapcho M. SEER cancer statistics review, 1975-2005. Bethesda (MD): National Cancer Institute; 2008. Available at: http://seer.cancer.gov/csr/1975_2005/.
Silverman S Jr, Gorsky M, Lozada F. Oral leukoplakia and malignant transformation: a follow-up study of 257 patients. Cancer. 1984;53(3):563-568. doi: 10.1002/1097-0142(19840201)53:3<563::aid-cncr2820530332>3.0.co;2-f.
Sol Silverman Jr., DDS, Richard D. Rozen, DDS. Observations on the clinical characteristics and natural history of leukoplakia. J Am Dent Assoc. 1968;76(4):772-777. doi: 10.14219/jada.archive.1968.0141.
Pindborg JJ, Reichart P, Smith CJ, van der Waal I (1997). World Health Organization: histological typing of cancer and precancer of the oral mucosa. Berlin: Springer-Verlag.
Axéll T, Pindborg JJ, Smith CJ, van der Waal I. Oral white lesions with special reference to precancerous and tobacco- related lesions: conclusions of an international symposium held in Uppsala, Sweden, May 18-21 1994. International Collaborative Group on Oral White Lesions. J Oral Pathol Med 1996;25(2):49- 54. doi: 10.1111/j.1600-0714.1996.tb00191.x.
Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45(4-5):309-316. doi: 10.1016/j.oraloncology.2008.06.002.
Thomas G, Hashibe M, Jacob BJ, Ramadas K, Mathew B, Sankaranarayanan R, Zhang ZF. Risk factors for multiple oral premalignant lesions. Int J Cancer. 2003;107(2):285-291. doi: 10.1002/ijc.11383.
Hashibe M, Mathew B, Kuruvilla B, Thomas G, Sankaranarayanan R, Parkin DM, et al. Chewing tobacco, alcohol, and the risk of erythroplakia. Cancer Epidemiol Biomarkers Prev. 2000;9(7):639-645.
CH Chung, YH Yang, TY Wang, TY Shieh, S Warnakulasuriya. Oral precancerous disorders associated with areca quid chewing, smoking, and alcohol drinking in southern Taiwan. J Oral Path and Med. 2005;34 (8):460-466. doij.1600-0714.2005.00332.x.
Isaäc van der Waal. Oral potentially malignant disorders: Is malignant transformation predictable and preventable. Med Oral Patol Oral Cir Bucal. 2014;19(4):e386–e390. doi: 10.4317/medoral.20205.
Jagtap SV, Warhate P, Saini N, Jagtap SS, Chougule PG. Oral premalignant lesions: a clinicopathological study. Int Sur J 2017;4(10):3477-3481. doi: 10.18203/2349-2902.isj20174520.
Bouquot, JE. Reviewing oral leukoplakia-clinical concepts for the 1990s. J Amer Dent Assoc. 1991;122(6):80-82. doi: 10.1016/s0002-8177(91)26024-9.
Starzyńska A, Pawłowska A, Renkielska D, Michajłowski I, Sobjanek M, Błażewicz I. Oral premalignant lesions: epidemiological and clinical analysis in the northern Polish population. Postepy Dermatol Alergol. 2014;31(6):341-350. doi: 10.5114/pdia.2014.40932.
Chung CH, Yang YH, Wang TY, Shieh TY, Warnakulasuriya S. Oral precancerous disorders associated with areca quid chewing, smoking, and alcohol drinking in southern Taiwan. J Oral Pathol Med. 2005;34(8):460-466. doi: 10.1111/j.1600-0714.2005.00332.x.
Silverman S, Gorsky M, Lozada F. Oral leukoplakia and malignant transformation. A follow-up study of 257 patients. Cancer. 1984;53(3):563-568. doi: 10.1002/1097-0142(19840201)53:3<563::aid-cncr2820530332>3.0.co;2-f.
Gowhar O, Ain TS, Singh NN, Sultan S. Prevalence of oral premalignant and malignant lesions in moradabad, India - A Retrospective Study. Int J Cont Med Res. 2016;3(7):2079- 2081.
Patil PB, Bathi B, Chaudhari S. Prevalence of oral mucosal lesions in dental patients with tobacco smoking, chewing, and mixed habits: A cross-sectional study in South India; J Fam and Com Med. 2013; 20(2): 130-135. doi: 10.4103/2230-8229.114777.
Kumar S, Debnath N, Ismail MB, Kumar A, Kumar A, Badiyani BK. Prevalence and Risk Factors for Oral Potentially Malignant Disorders in Indian Population; Adv Prev Med. 2015; 2015: 208519. doi: 10.1155/2015/208519.
Mehta FS, Sahiar BE, Daftary DK, Gupta PC, Pindborg JJ. A correlative histocytological study of carcinoma and epithelial atypia of the palate among Indian reverse smokers. Br J Cancer. 1972;26(3):230-233. doi: 10.1038/bjc.1972.31.
Vincent SD, Fotos PG, Baker KA, Williams TP. Oral lichen planus: the clinical, historical, and therapeutic features of 100 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1990;70(2):165-171. doi: 10.1016/0030-4220(90)90112-6.z.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

