Clinical profile & visual outcome in ocular chemical injury
Abstract
Objective: To study the clinical profile & visual outcome of ocular chemical injuries.
Material & Method: The cases of ocular chemical injury were included in the study. Detailed history of the patients was taken pertaining to the injury. The ocular examination was performed visual acuity was recorded by using Snellen’s test type Chart. A thorough examination was carried out on slit-lamp, direct & indirect ophthalmoscope. Clinical grading was done by Roper Hall Classification. Other ocular investigations were done when required.
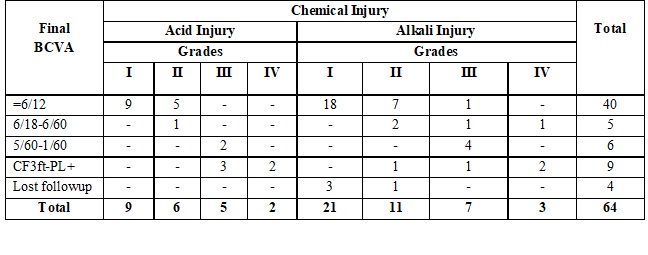
Results: The present study included 64 eyes of 54 patients, of which 80% (43) were male and 20% (11) females. The mean age was 22 ±13 yrs. higher prevalence 66% of chemical ocular injury was seen in lower socioeconomic group. Alkali injuries (66%) were more common than acid injuries (34%). Calcium carbonate (lime) 31% was the most common etiological agent. Most chemical injuries were unilateral 81% Maximum no. of patients belongs to grade I (48%) and minimum in grade IV (8%). In grade I chemical injury, most patients were presented with visual acuity better than 6/12. The final visual acuity is dependent on the initial grading and vision, higher the grade lesser are the chances of significant visual improvement.
Conclusion: Presenting visual acuity is an important prognostic factor. Lower grades of injury had better final visual outcome. Grade III and grade IV alkali injuries are more severe injuries than acids.
Downloads
References
2. Liggett PE, Pince KJ, Barlow W, et al. Ocular trauma in an urban population. Review of 1132 cases. Ophthalmology. 1990 May;97(5):581-4.[pubmed]
3. Macewen CJ. Eye injuries: a prospective survey of 5671 cases. Br J Ophthalmol. 1989 Nov;73(11):888-94. DOI:10.1136/bjo.73.11.888.[pubmed]
4. Zagelbaum BM, Tostanoski JR, Kerner DJ, et al. Urban eye trauma. A one-year prospective study. Ophthalmology. 1993 Jun;100(6):851-6.[pubmed]
5. Morgan SJ. Chemical burns of the eye: causes and management. Br J Ophthalmol. 1987 Nov;71(11):854-7. DOI:10.1136/bjo.71.11.854.[pubmed]
6. Pfister R.R., Pfister D.R. Alkali injuries of the eye. In: Krachmer J.H., Mannis M.J., Holland E.J., ed. Cornea, Philadelphia: Elsevier Mosby; 2005:1285-9.3
7. Pfister RR, Friend J, Dohlman CH. The anterior segments of rabbits after alkali burns. Metabolic and histologic alterations. Arch Ophthalmol. 1971 Aug;86(2):189-93. DOI:10.1001/archopht.1971.01000010191013.[pubmed]
8. Paterson C.A., Pfister R.R., Levinson R.A. Aqueous humor pH changes after experimental alkali burns. Am J Ophthalmol 1975; 79:414-9.[pubmed]
9. McCulley JP. Ocular hydrofluoric acid burns: animal model, mechanism of injury and therapy. Trans Am Ophthalmol Soc. 1990;88:649-84.[pubmed]
10. McCulley J.P. Chemical injuries. In: Smolin G., Thoft R.A., Ed. The cornea: scientific foundation and clinical practise, Boston: Little, Brown and Co; 1987:527-42.
11. Friedenwald J.S., Hughes W.F., Herrmann H.: Acid injuries of the eye. Arch Ophtalmol Rev Gen Ophtalmol 1946; 35:98-108.
12. Schirner G., Schrage N.F., Salla S., et al: Conjunctival tissue examination in severe eye burns: a study with scanning electron microscopy and energy-dispersive X-ray analysis. Graefes Arch Clin Exp Ophthalmol 1995; 233:251-6.
13. Wagoner MD. Chemical injuries of the eye: current concepts in pathophysiology and therapy. Surv Ophthalmol. 1997 Jan-Feb;41(4):275-313.[pubmed]
14. Kuckelkorn R, Luft I, Kottek AA, et al. Chemical and thermal eye burns in the residential area of RWTH Aachen. Analysis of accidents in 1 year using a new automated documentation of findings. KlinMonbl Augenheilkd. 1993 Jul;203(1):34-42. DOI:10.1055/s-2008-1045646.[pubmed]
15. Parul Singh, Manoj Tyagi, Yogesh Kumar, K. K. Gupta, P. D. Sharma. Ocular chemical injuries and their management; Oman J Ophthalmol. 2013; 6(2): 83–6.
16. Haring RS, Sheffield ID, Channa R, et al. Epidemiologic Trends of Chemical Ocular Burns in the United States. JAMA Ophthalmol. 2016 Oct 1;134(10):1119-1124. doi: 10.1001/jamaophthalmol.2016.2645.[pubmed]
17. Adepoju FG, Adeboye A, Adigun IA. Chemical eye injuries: presentation and management difficulties. Ann Afr Med. 2007 Mar;6(1):7-11.[pubmed]
18. Vajpayee RB, Shekhar H, Sharma N, et al. Demographic and clinical profile of ocular chemical injuries in the pediatric age group. Ophthalmology. 2014 Jan;121(1):377-380. doi: 10.1016/j.ophtha.2013.06.044. Epub 2013 Aug 12.
19. Midelfart A, Hagen YC, Myhre GB. [Chemical burns to the eye]. Tidsskr Nor Laegeforen. 2004 Jan 8;124(1):49-51.[pubmed]
20. Sher LM, Taylor DM, Robinson J, Browning J, Colbridge M, Macleod D, McCracken H, McKenzie C. Surveillance of severe chemical corneal injuries in the UK. Br J Ophthalmol. 2009 ;93(9):40-3.
Copyright (c) 2019 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

