A prospective study of prevalence and types of leprosy with ocular lesions
Abstract
Introduction: Leprosy (Hansen disease) is a chronic infectious disease caused by an intracellular acid-fast bacillus Mycobacterium leprae which apart from skin, nasal mucosa and peripheral nerves also affects the anterior segment of the eye.M.leprae was discovered over a hundred years ago (around 1873) by Armauer Hansen. It is a disease that does not kill the affected individual but cripples. When the threat of blindness is also added to patient’s natural dread of the disease, the condition is indeed terrifying.
Materials and methods: This study comprises of detailed examination of 180 consecutive patients of Hansen's disease. It has been carried out in the Department of Ophthalmology, Mamata General Hospital, Khammam and with the cooperation of department of Dermatology, Mamata General Hospital.Allpatients who were admitted inthe leprosy department with leprosy from 2015 January to December 2016 December were included in this study.All the patients withcongenital abnormalities, inflammatory conditions of the breast and breast carcinomas were excludedfrom the study.
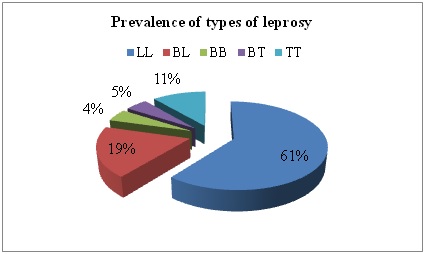
Results: This study includes a total number of 180 patients of leprosy disease who were carefully examined for any evidence of ocular lesion. Most of the patients were males, females accounting for only 21.79%. Among the 180 patients, 60 patients had the evidence of the ocular involvement. It points out to the fact that most of the Hansen's patients develop ocular lesions.
Conclusion: Most of the patients are adults. There is no significant influence of age either on the presence or absence of eye involvement or in the type of Hansen's disease.The commonest type of leprosy is lepromatous leprosy followed by all types of borderline leprosy. The incidence of ocular involvement is very high in these two forms of leprosy disease (86.6%& 63.6%).
Downloads
References
2. Sharma A, Sharma RK, Goswsami KC, Bardwaj S. Clinico-Histopathological Correlation in Leprosy. JK Science. 2008;10:120–3.
3. Shenoi SD, Siddappa K. Correlation of clinical and histopathologic features in untreated macular lesions of leprosy: A study of 100 cases. Ind J Lepr. 1988;60:202–6.
4. Nadkarni NS, Rege VL. Significance of histopathological classification in leprosy. Ind J Lepr. 1999;7:325–32.[pubmed]
5. Moorthy BN, Kumar P, Chatura KR, Chandrasekhar HR, Basavaraja PK. Histopathological correlation of skin biopsies in leprosy. Ind J Dermatol Ven Leprol. 2001;67:299–301.[pub med]
6. V Pannikar VK, Arunthathi S, Chacko CJ, Fritschi EP. A clinicopathological study of primary neuritic leprosy. Ind J Lepr. 1983;55:212–21.[pubmed]
7. Jacob M, Arunthathi S. The Wague; 1988. A study of primary neuritic leprosy (Abst): In Proc XIII Int LepCongr (September 11-17) p. 313.
8. Girdhar BK. Neuritic leprosy. Indian J Lepr. 1996;68:35–42.[pubmed]
9. Enhanced Global Strategy for Further Reducing the Disease Burden due to Leprosy (Plan Period: 2011-2015) World Health Organization, SEA-GLP-2009.3
10. Singh K, Iyengar B, Singh R. Variation in clinical and histopathological classification of leprosy: A report and plausible explanation. Lepr India. 1983;55:472–9.
11. Kalla G, Salodkar A, Kachhawa D. Clinical and histopathological correlation in leprosy. Int J Lepr. 2000;68:184–5.[pubmed]
12. Shanker Narayan NP, Ramu G, Desikan KV, Vallishayee RS. Correlation of clinical, histological and immunological features across the leprosy spectrum. Ind J Lepr. 2001;73:329–42.
13. Singhi MK, Kachhawa D, Ghiya BC. A retrospective study of clinico-histological correlation in leprosy. Ind J Pathol Microbiol. 2003;46:47–8.
14. Kaur S, Sharma VK, Basak P, Kaur I. Paucibacillary multidrugtherapy in leprosy: 7 1/2 year experience. Ind J Lepr. 1992;64:153–61.[pubmed]
15. Singh RP, Tiwari VD, Chattopadhyay SP. Comparative study of short-term results in two multidrug regimens in MB leprosy. Ind J Lepr. 1993;65:173–80.[pubmed]
16. Kishore BN, Shetty JN. Bacterial clearance with WHO recommended MDR for MB leprosy. Ind J Lepr. 1995;67:301–8.[pubmed]
17. Shivayogi R. Kusagur, Mamatha S. Kusagur, Gururaj K. J. “A clinical study of ocular manifestations in leprosy”. Journal of Evolution of Medical and Dental Sciences 2013; Vol2, Issue 36, September 9; Page: 6816-6823.
18. Lewallen, Paul Courtright. An overview of ocular leprosy after 2 decades of multidrug therapy. International ophthalmology clinics – world blindness. Sep 2004, Vol-47; No. (3):8799.
19. Sihota. Tandon Disease of the uveal tract chapter 17. Parsons disease of the eye 20thedn. New Delhi Elsevier 2007; 239-72.
20. Dr. MargreetHogeweg, Dr Murray McGavin, Prevention of Blindness Due To Leprosy. ICEH, http://www.iceh.org.uk.Indian association of Leprologists-approved classification. Lepr India. 1982;54:22–32.
21. WHO Tech Rep Ser 675. Geneva: WHO; 1982. World Health Organizion. Chemotherapy of leprosy for control programmes. Geneva: WHO; 1988. WHO Expert Committee Report on Leprosy. Sixth Report. TRS 768.
22. Sachdeva S, Amin SS, Khan Z, Alam S, Sharma PK. Childhood leprosy: A retrospective study. J Public Health Epidemiol. 2010;2:267–71.
Copyright (c) 2019 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

