INCREASED INCIDENCE OF RHINO-ORBITAL MUCORMYCOSIS IN AN EDUCATIONAL THERAPEUTIC HOSPITAL DURING THE COVID-19 PANDEMIC: AN OBSERVATIONAL STUDY.
RHINO-ORBITAL MUCORMYCOSIS
Abstract
ABSTRACT
Introduction: Coronavirus had become an emergency in 2019. At that time invasive mucormycosis post-COVID-19 also emerged. There are multiple case reports and case series describing mucormycosis in COVID-19. The recent emergence of the Coronavirus Disease (COVID-19) disease had been associated with reports of fungal infections such as aspergillosis and mucormycosis especially among critically ill patients like immune-compromised patients who have been treated with steroids.
Aim: The aim of the study was to find out the clinical features, risk factors, and outcomes of patients with coronavirus disease 2019 (COVID-19)-associated mucormycosis (CAM).
Method: A cross-sectional was conducted on patients with MRI and biopsy-proven mucormycosis with RT-PCR-confirmed COVID-19 from May to August 2021 at Dr. D. Y. Patil Medical College and Research Institute, kadamwadi, Kolhapur, Maharashtra, India. the time interval between COVID-19 and mucormycosis, underlying systemic diseases, clinical features, course of the disease, and outcomes were collected and analysed. (n=32)
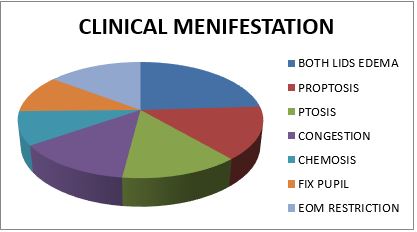
Result: out of 45 mucormycosis patients, 10 were female and 35 were male. The youngest participant was aged 12 years, and the oldest was 75 years old, the mean age was 53.33 ± 14.99 years. The majority of patients, 27 (60%) are diabetic and 10 are hypertensive (22.22%). 28 patients were COVID-19 positive. And 66.67% of patients were rhino orbital type of mucormycosis. All patients were treated with amphotericin-B but out of 11(24.44%) got transcutaneous retrobulbar amphotericin –B injection.
Conclusion: SARS-COV-2 infected patient numbers were increasing in COVOD -19 pandemic. Mucormycosis proved itself an epidemiological burden. So risk-based approach for patients with risk is necessary. Attention was to be given to that patients who were diabetic (uncontrolled sugar level), on combined use of steroids, or on immune-modulating agents.
Downloads
References
1) Al-Tawfiq JA, Alhumaid S, Alshukairi AN, Temsah MH, Barry M, Al Mutair A, Rabaan AA, Al-Omari A, Tirupathi R, AlQahtani M, AlBahrani S. COVID-19 and mucormycosis superinfection: the perfect storm. Infection. 2021 Oct; 49:833-53.
2) Sundaram N, Bhende T, Yashwant R, Jadhav S, Jain A. Mucormycosis in COVID-19 patients. Indian Journal of Ophthalmology. 2021 Dec;69(12):3728.
3) Ajith Kumar AK, Gupta V. Rhino orbital cerebral mucormycosis. StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
4) Veisi A, Bagheri A, Eshaghi M, Rikhtehgar MH, Rezaei Kanavi M, Farjad R. Rhino orbital mucormycosis during steroid therapy in COVID 19 patients: A case report. Eur J Ophthalmol 2021; 11206721211009450.doi: 10.1177/11206721211009450. Online ahead of print.
5) Maini A, Tomar G, Khanna D, Kini Y, Mehta H, Bhagyasree V. Sino orbital mucormycosis in a COVID 19 patient: A case report. Int J Surg Case Rep 2021; 82:105957.
Copyright (c) 2023 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

