Retrospective study on middle ear risk indices in analyzing postoperative outcome following tympanoplasty
Abstract
Introduction
Middle Ear Risk Index (MERI) of a patient suffering from Chronic otitis media (COM) is a numerical grading to stratify the severity of disease. The aim of study was to evaluate MERI in the post operative outcome following tympanoplasty in terms of hearing improvement and graft uptake.
Materials and Methods
A retrospective study on patients with COM undergoing tympanoplasty within the age group 15-50 from February 2017 - February 2018 was done. Data was collected from the medical records department through case sheets. Graft uptake status at the end of one month was obtained from minor register. Post operative Audiograms done at end of 3 months were obtained from the Audiology Database.
Results
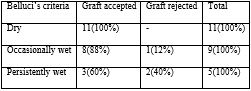
25 patients with unilateral perforation were operated and followed up in this time period. There were 11 male and 14 female patients. 88% patients had mild MERI score, 8% had moderate and 4% had severe MERI scores. About 84% had mild conductive hearing loss while rest had moderate hearing loss. Graft acceptance was 88%, it was 95% in mild MERI and 50% in moderate MERI groups respectively. In occasionally wet ears graft rejection was 11% and 40% in persistently wet ears. The mean preoperative Air-Bone gap in the Mild MERI and Moderate MERI group were 21.45 decibel (dB) and 22.3 dB. The mean post- operative Air-Bone gap in the Mild MERI risk group was 10.35 dB and 14.5 dB in the moderate MERI risk group which was significant(p<0.05).
Conclusion
Hence MERI index is a very useful predictor of graft uptake and audiological gain in patients undergoing tympanoplasty surgeries.
Downloads
References
2. Tos M. Late Results in Tympanoplasty. Staging the operation. Acta Oto- La-ryngologica. 1976; 82(1): 282-285.
3. Hirsch BE, Kamerer DB, Doshi S. Single Stage Management of Cholesteatoma. Otolaryngology Head and Neck Surgery. 1992; 106(4): 351-354.
4. Sheehy JL, Crabtree JA. Tympanoplasty: Staging the Operation. Laryngoscope. 1973; 83(10): 1594-1621. doi: 10.1288/00005537-197310000-00003
5. Shelton C, Sheehy JL. Tympanoplasty: Review of 400 Staged Cases. Laryngoscope. 1990; 100(7): 679-681. doi: 10.1288/00005537-199007000-00001
6. Black B. Ossiculoplasty prognosis: the spite method of assessment. Am J Otol. 1992; 13: 544-551.
7. Albu S, Babighian G, Trabalzini F. Prognostic factors in tympanoplasty. The American Journal of otology. 1998; 19: 136-140.
8. Brackman DE, Sheehy JL, Luxford WM. TORPs and PORPs in tympanoplasty: a review of 1042 operations. Otolaryngol Head Neck Surg. 1984; 92: 32-37.
9. Kartush JM. Ossicular chain reconstruction. Capitu-lum to Malleus. Otolaryngol Clin North Am. 1994; 27(4): 689-715.
10. Wasson JD, Papadimitriou CE, Pau H. Myringoplasty: impact of perforation size on closure and audiological improvement. J Laryngol Otol. 2009; 123: 973-977. doi: 10.1017/S0022215109004368
11. Pignataro L, Berta LGD, Capaccio P, Zaghis A. Myringoplasty in children: anatomical and functional results. J Laryngol Otol. 2001; 115: 369-373.
12. Holmquist I. The role of eustachian tube in the myringoplasty. Acta Otolaryngol (stockh). 1968; 66: 289.
13.Shishegar M, Faramarzi M, Rashidi Ravari M. Evaluation of middle ear risk index in patients undergoing tympanoplasty. Eur Arch Otorhinolaryngol. 2019 Oct;276(10):2769-2774. doi: 10.1007/s00405-019-05539-w. Epub 2019 Jul 17. PMID: 31317321 (for meri )
14. Onal K, Uguz MZ, Kazikdas KC, Gursoy ST, Gokce H. A multivariate analysis of otological, surgical and patient‐related factors in determining success in myringoplasty. Clinical Otolaryngology. 2005;30(2):115–20.
15. Emir H, Ceylan K, Kizilkaya Z, Gocmen H, Uzunkulaoglu H, Samim E. Success is a matter of experience: type 1 tympanoplasty. European archives of otorhinolaryngology. 2007;264(6):595–9.
16. Lima JCBD, Marone SAM, Martucci O, Gonçalez F, Silva Neto JJD, Ramos ACM. Evaluation of the organic and functional results of tympanoplasties through a retro-auricular approach at a medical residency unit. Brazilian journal of otorhinolaryngology. 2011;77(2):229–36.
17. Sharma, A., Saxena, R., Verma, L., & Bhandari, S. Correlation Between MERI and Hearing After Tympanoplasty. Journal Of Nepalgunj Medical College.2017; 13(2):6-9.
18. Ahmed A, Sharma SC. Middle Ear Risk Index [MERI] as Prognostic Factor in Tympanomastoidectomy with Tympanoplasty. Madridge J Otorhinolaryngol. 2016; 1(1): 15-22.
19. Kumar N, Madkikar NN, Kishve S, Chilke D, Shinde KJ. Using Middle Ear Risk Index and ET Function as Parameters for Predicting the Outcome of Tympanoplasty. Indian Journal of Otolaryngology and Head & Neck Surgery. 2012;64(1):13-16. doi:10.1007/s12070-010-0115-4.
20. Pinar E, Sadullahoglu K, Calli C, Oncel S. Evaluation of prognostic factors and middle ear risk index in tympanoplasty. Otolaryngology-Head and Neck Surgery. 2008;139(3):386–90.
21. Naderpour M, Jabbari Moghadam Y, Ghanbarpour E, Shahidi N. Evaluation of Factors Affecting the Surgical Outcome in Tympanoplasty. Iranian Journal of Otorhinolaryngology. 2016;28(85):99-104.
22. Becvarovski Z, Kartush JM. Smoking and tympanoplasty: implications for prognosis and the Middle Ear Risk Index (MERI) The Laryngoscope. 2001;111(10):1806–11.
Copyright (c) 2022 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

