A Prospective Study to Analyse the Post-Operative Outcome ofSutureless and Glueless Pterygium Autograft Surgery
Abstract
Background: The present study was conducted to study the incidence of recurrence afterpterygium excision followed by glueless and sutureless implantation of conjunctival autograft and tostudy the outcome of surgery in terms of graft positioning.
Material and Methods: This study wasconducted as a prospective study on 47 patients presenting with pterygium at a tertiary care centreduring the study period of 2 years. Detailed ocular and systemic examinations were done. Patientswere then subjected to pterygium excision followed by glueless and sutureless implantation ofconjunctival autograft. The patients were followed up at 48 hrs after the surgery, then at the firstweek, the first month, third-month sixth month to assess the positioning of the graft, signs ofrecurrence if any (neovascularization, formation of early pterygium tissue).
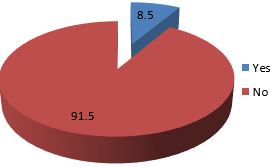
Results: The study wasconducted on a total of 47 patients with pterygium with a mean age of 46.51±15.28 years. Themajority of patients belonged to 51 to 60 years of age (31.9%). Male predominance for pterygiumwith a male: female ratio of 1.6:1 was observed. Majority of patients presented with grade 3pterygium. Recurrence of pterygium and neovascularisation was observed in 8.5% of patients. Graftdisplacement was observed in 17% of patients.
Conclusion: Sutureless glueless pterygiumautograft surgery is a safe procedure with less operative time and postoperative complications. Therecurrence rate and risk of neovascularization are low but the incidence of graft failure is one of themajor drawbacks of this procedure.
Downloads
References
2. Duke-Elder S. Leigh AG. in: Duke-Elder S (Eds.)., System of Ophthalmology, Vol.8, Henry Kimpton Publishers, London 1965, pp. 573-585
3. Notara M, Lentzsch A, Coroneo M, Cursiefen C. The role of limbal epithelial stem cells in regulating corneal (lymph) angiogenic privilege and the micromilieu of the limbal niche following UV exposure. Stem cells international. 2018 May 8;2018.
4. Di Girolamo N, Chui J, Coroneo MT, Wakefield D. Pathogenesis of pterygia: role of cytokines, growth factors, and matrix metalloproteinases. Progress in retinal and eye research. 2004 Mar 1;23(2):195-228.
5. Mathur ML, Haldiya KR, Sachdev R, Saiyed HN. The risk of pterygium in salt workers. International ophthalmology. 2005 Apr 1;26(1-2):43-7.
6. Gupta VP. Conjunctival transplantation for pterygium. DJo. 1997;5:5-12.
7. Bhatia J, Varghese M, Narayanadas B, Bhatia A. Cut-and-place technique of pterygium excision with autograft without using sutures or glue: Our experience. Oman journal of ophthalmology. 2017 May;10(2):81.
8. Liang W, Li R, Deng X. Comparison of the efficacy of pterygium resection combined with conjunctival autograft versus pterygium resection combined with amniotic membrane transplantation. Eye science. 2012 Jun 1;27(2):102-5.
9. Yu C, Liang W, Huang Y, Guan W. Comparison of clinical efficacy of three surgical methods in the treatment of pterygium. Eye science. 2011 Dec 1;26(4):193-6.
10. Foroutan A, Beigzadeh F, Ghaempanah MJ, Eshghi P, Amirizadeh N, Sianati H, Foroutan P. Efficacy of autologous fibrin glue for primary pterygium surgery with conjunctival autograft. Iran J Ophthalmol. 2011, 23:39-47.
11. de Wit D, Athanasiadis I, Sharma A, Moore J. Sutureless and glue-free conjunctival autograft in pterygium surgery: a case series. Eye. 2010 Sep;24(9):1474-7.
12. Kulthe SB, Bhosale AP, Patil PU, Pandve HT. Is the surgical technique of a sutureless and glue-free conjunctivolimbal auto graft after pterygium excision complications free?. Med J DY PatilUniv 2015;8:308-12
13. Dorfman HS, Kennedy JE, Bird WC. Longitudinal evaluation of free autogenous gingival grafts. Journal of clinical periodontology. 1980 Aug;7(4):316-24.
14. Gupta R. Outcome of Sutureless and Glue free Conjunctival Autograft in primary pterygium Surgery. J. of. Med Sci&Clin Res. 2018. 6 (12);503-7.
15. Singh PK, Singh S, Vyas C, Singh M. Conjunctival autografting without fibrin glue or sutures for pterygium surgery. Cornea 2013;32:104-7
16. Rangu RV, Wanjari A, Akhade N. Study of sutureless and glue-free conjunctival autograft. International Journal of Recent Trends in Science And Technology 2014;10:480-82.
17. Bhargava P, Kochar A, Joshi R. A novel technique–Pterygium excision followed by sutureless and gluefree conjunctival autografting. ActaMedica Scientia. 2015;2:6.
18. Malik KP, Goel R, Gupta A, Gupta SK, Kamal S, Malik VK, Singh S. Efficacy of sutureless and glue free limbal conjunctival autograft for primary pterygium surgery. Nepalese Journal of Ophthalmology. 2012 Jul 25;4(2):230-5.
19. Sarkar S. Pterygium Excision with Conjunctival Autograft Without Suture without Glue.IOSR-JDMS 16: 82-86.
20. Dasgupta S, Vats V, Mittal SK. Pterygium excision with suture-free, glue-free conjunctival autograft (SFGF-CAG): Experience of a tertiary care hospital of the Northern India. Journal of Clinical Ophthalmology and Research. 2016 Sep 1;4(3):143.
Copyright (c) 2022 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

