Congenital Dacryocystitis- Clinical Profile and Outcome
Abstract
Aim: To assess the clinical and epidemiological profile of congenital dacryocystis and its treatment outcome.
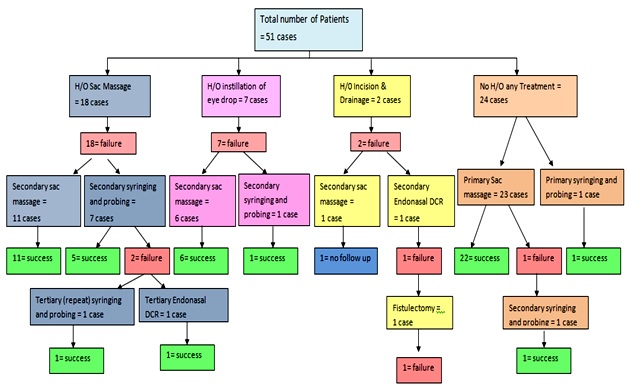
Material and Methods: A prospective study was conducted for duration of two years, cases with congenital dacryocystitis of age less than 5 years were included. A detailed history was taken giving emphasis to epiphora onset, duration, treatment and resolution. Ocular examination was done along with regurgitation on pressure over lacrimal sac test. The plan for the management was standard stepwise approach according to age groups and clinical condition of the cases. The conservative treatment included sac massage and surgical procedure were probing and syringing and endonasal dacryocystorhinostomy. Follow-up was done for 6 months and final clinical assessment was done to assess the success of procedure.
Results: Total 65 eyes of 51 cases were included in the study. Mean age of presentation was- 14.6 ± 2.3 months with 52.9% females. Unilateral involvement was more common. Epiphora was most common complaint with 63% ROPLAS positive. The success rate of sac massage was 81% and the overall success rate for treatment of congenital dacryocystitis was 96%.
Conclusion: Congenital dacryocystitis is a common pediatric problem. Treatment of congenital dacryocystitis should be started as early as possible and in stepwise manner initially conservative than surgical.
Downloads
References
2. GUERRY D 3rd, KENDIG EL Jr. Congenital impatency of the nasolacrimal duct. Arch Ophthal. 1948 Feb;39(2):193-204.[pubmed]
3. Kushner BJ. Congenital nasolacrimal system obstruction. Arch Ophthalmol. 1982 Apr;100(4):597-600.[pubmed]
4. Crigler L: The treatment of congenital dacryocystitis. JAMA 1923; 81:23–4.
5. Albert and jakobiec’s ophthalmology- principle and practice of ophthalmology 3rd edition; February 12, 2008 volume-3; 3503-18.
6. Robb RM. Probing and irrigation for congenital nasolacrimal duct obstruction. Arch Ophthalmol. 1986 Mar;104(3):378-9.[pubmed]
7. Jack J Kanski Brad Bowling- clinical ophthalmology a systematic approach – 7th edition; 2011; Elsevier Limited. 72-78
8. Aldahash FD, Al-Mubarak MF, Alenizi SH, Al-Faky YH. Risk factors for developing congenital nasolacrimal duct obstruction. DOI:10.1016/j.sjopt.2013.09.007.[pubmed]
9. Shivpuri D, Puri A. Congenital nasolacrimal duct obstruction: the proper technique of massage. Indian Pediatr. 1994 Mar;31(3):337-40.[pubmed]
10. Kakizaki H, Takahashi Y, Kinoshita S, Shiraki K, IwakiMThe rate of symptomatic improvement of congenital nasolacrimal duct obstruction in Japanese infants treated with conservative management during the 1st year of age. Clin Ophthalmol. 2008; 2(2): 291–4.
11. Abrishami M, BagheriA,HosseinS S, Mirdehghan S. A. Late Probing for Congenital Nasolacrimal Duct Obstruction. J of Ophthalmic & Vision Research 2009;4(2):102-4.
12. Wang JC, Cunningham MJ. Congenital dacryocystocele: is there a familial predisposition? DOI:10.1016/j.ijporl.2010.11.026.[pubmed]
13. Bhardwaj P, Singh K, Sharma K, Chalia D, Pal S. Lacrimal syringing versus combined lacrimal probing and syringing for treatment of congenital nasolacrimal duct obstruction in children. Int J Med Res Rev 2016;4 (6):964-970.
14. Kim HC, Cho AR, Lew H. Dacryoscintigraphic findings in the children with tearing. DOI:10.3341/kjo.2015.29.1.1.[pubmed]
15. Cha SD, Lee H, Park M S, Lee J M, Baek S H. Clinical Outcomes of Initial and Repeated Nasolacrimal Duct Office-Based Probing for Congenital Nasolacrimal Duct Obstruction.Korean Journal of Ophthalmology 2010;24(5):261-6
16. Casady DR, Meyer DR, Simon JW, et al. Stepwise treatment paradigm for congenital nasolacrimal duct obstruction.DOI:10.1097/01.iop.0000225750.25592.7f.[pubmed]
17. Pediatric Eye Disease Investigator Group. Resolution of congenital nasolacrimal duct obstruction with nonsurgical management.DOI:10.1001/archophthalmol.2012.454.[pubmed]
18. Kakizaki H, Takahashi T, Kinoshita S, Shiraki K, Iwaki M. The rate of symptomatic improvement of congenital nasolacrimal duct obstruction in Japanese infants treated with conservative management during the first year of age. Clin Ophthalmol. 2008;2: 291–294.
19. Serin, Didem Buttanri, Ibrahim Bulent et alPrimary probing for congenital nasolacrimal duct obstruction with manually curved Bowman probes Clinical Ophthalmology. 2013;7:109-112
20. Kim YS, Moon SC, Yoo KW. Congenital nasolacrimal duct obstruction: irrigation or probing? DOI:10.3341/kjo.2000.14.2.90.[pubmed]
21. Kashkouli MB, Kassaee A, TabatabaeeZ.Initial nasolacrimal duct probing in children under age 5: cure rate and factors affecting success. J AAPOS.2000; 6: 360–3.[pubmed]
22. Kashkouli MB, Beigi B, Parvaresh MM, et a. Late and very late initial probing for congenital nasolacrimal duct obstruction: what is the cause of failure? Br J Ophthalmol. 2003 Sep;87(9):1151-3.[pubmed]
23. Maheshwari R. Results of probing for congenital nasolacrimal duct obstruction in children older than 13 months of age. Indian J Ophthalmol. 2005 Mar;53(1):49-51.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.

 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

