Hyperthyroidism associated with intraocular pressure and dry eye
Abstract
Introduction: Graves’ orbitopathy/ophthalmopathy (GO) also known as thyroid eye disease (TED), dysthyroid/thyroid-associated ophthalmopathy (TAO), is an autoimmune disorder representing the commonest and most important extrathyroidal manifestation of Graves’ disease.
Materials and Methods: This is a prospective study conducted for 2 years. A total of 60 established cases of Hyperthyroidism of all Age groups with either gender subjects who were diagnosed with Thyroid orbitopathy at hospitals were included in this study. History of ocular surgery or medications, those demonstrating the recent use of contact lenses, pregnant or lactating women. All the cases with similar presentation not proved to be Thyroid Orbitopathy and patients who did not report for the follow-up were excluded from the study.
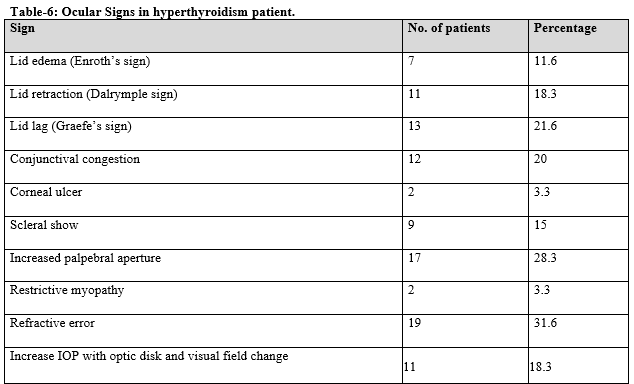
Result: A total of 60 patients were examined. Of the 60 cases analyzed, female preponderance was noted and 41-60 years age group had the highest incidence of thyroid orbitopathy. The most common presentation was found to be unilateral. Inferior rectus muscle was the commonest muscle involved with 48.3% followed by Medial rectus muscle 38.3%, Superior rectus muscle 23.3%, and Lateral rectus muscle involved least with 11.6% in descending order. None of the patients reported a loss of vision.
Conclusions: Dry eye and increased IOP have commonly seen outcomes that should be managed diligently. This potential sight-threatening condition is seen worldwide and has many functional and cosmetic consequences that need to be recognized. Hyperthyroidism was significantly associated with the severity.
Downloads
References
Lee HB, Rodgers IR, Woog JJ. Evaluation and management of graves’ orbitopathy. Otolaryngol Clin North Am. 2006;39(5):923-942. doi: 10.1016/j.otc.2006.07.008.
Zhang J, Lazar MA. The mechanism of action of thyroid hormones. Annu Rev Physiol. 2000;62:439-66. doi: 10.1146/annurev.physiol.62.1.439.
Metcalfe RA, Weetman AP. Stimulation of extraocular muscle fibroblasts by cytokines and hypoxia: Possible role in thyroid-associated ophthalmopathy. Clin Endocrinol (Oxf). 1994;40(1):67-72. doi: 10.1111/j.1365-2265.1994.tb02445.x.
Feely J, Isles TE. Screening for thyroid dysfunction in diabetics. Br Med J. 1979;1(6179):1678. doi: 10.1136/bmj.1.6179.1678.
Bartley GB, Fatourechi V, Kadrmas EF, Jacobsen SJ, Ilstrup DM, Garrity JA, et al. Chronology of graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol. 1996;121(4):426-434. doi: 10.1016/s0002-9394(14)70439-8.
Palikhe S, Thakur A, Narayan SD, Sharma AK, Acharya N. Ocular manifestations in thyroid eye disorder: A cross-sectional study from Nepal. Int J Clin Med. 2016;7(12):814-823. doi: 10.4236/ijcm.2016.712088
Woo KI, Kim YD, Lee SY. Prevalence and risk factors for thyroid eye disease among Korean dysthyroid patients. Korean J Ophthalmol. 2013;27(6):397-404. doi: 10.3341/kjo.2013.27.6.397.
Manji N, Carr-Smith JD, Boelaert K, Allahabadia A, Armitage M, Chatterjee VK, et al. Influences of age, gender, smoking, and family history on autoimmune thyroid disease phenotype. J Clin Endocrinol Metab. 2006;91(12):4873-4880. doi: 10.1210/jc.2006-1402.
Kashkouli MB, Pakdel F, Kiavash V, Heidari I, Heirati A, Jam S, et al. Hyperthyroid vs hypothyroid eye disease: The same severity and activity. Eye (Lond) 2011;25(11):1442-1446. doi: 10.1038/eye.2011.186
Saks ND, Burnstine MA, Putterman AM. Glabellar rhytids in thyroidassociated orbitopathy. Ophthalmic Plast Reconstr Surg. 2001;17(2):91-95. doi: 10.1097/00002341-200103000-00003.
Jarusaitiene D, Verkauzskiene R, Jasinskas V, Jankauskiene VJ. Predictive factors of development of graves’ ophthalmopathy for patients with juvenile graves’disease. Int J Endocrinol 2016;2016:9. doi: 10.1155/2016/8129497.
Cross JM, Girkin CA, Owsley C, McGwin G Jr. The association between thyroid problems and glaucoma. Br J Ophthalmol. 2008;92(11):1503-1505. doi: 10.1136/bjo.2008.147165.
Sultana S, Wadud SA, Huda S, Ahmed S. Open angle glaucoma and glaucoma suspect and ocular hypertension in thyroid related immune orbitopathy and thyroid disease. Bangabandhu Sheikh Mujib Med Univ J. 2015;8(1):50-55. doi: 10.3329/bsmmuj.v8i1.28921.
Bartalena L, Tanda ML. Graves' ophthalmopathy. New Eng J Med. 2009;360(10):994-1001. doi: 10.1056/NEJMcp0806317.
Etezad-Razavi M, Aboutorabi RB, Zarei-Ghanavati S, Daneshvar R. Prevalence and severity of ophthalmic manifestations of Graves' disease in Mashhad university endocrine clinics. Iran J Ophthalmol. 2006;19(3):14-21.
Cockerham KP, Pal C, Jani B, Wolter A, Kennerdell JS. The prevalence and implications of ocular hypertension and glaucoma in thyroid-associated orbitopathy. Ophthalmol. 1997;104(6):914-917. doi: 10.1016/s0161-6420(97)30207-3.
Jankauskiene J, Jakstaite V, Smalinskas V. Changes of vision and refraction in patients with thyroid pathology. Medicina (Kaunas). 2009;45(5):378-81.
Haefliger I, von Arx G, Pimentel AR. Pathophysiology of intraocular pressure increase and glaucoma prevalence in thyroid eye disease: a mini-review. Klin Monatsbl Augenheilkund. 2010;227(4):292-293. doi: 10.1055/s-0029-1245199.
Besharati M, Rastegar A. Clinical study of ophthalmopathy in patients with Graves’ disease. Asian J Ophthalmol. 2005;7(3):108-112.
Perros P, Neoh C, Dickinson J. Thyroid eye disease. BMJ. 2009;338: b560. doi: 10.1136/bmj.b560.
Lee A, Rochtchina E, Wang J, Healey PR, Mitchell P. Open-angle glaucoma and systemic thyroid disease in an older population. The Blue Mountains Eye Study. Eye Lond) 2004;18(6):600-608. doi: 10.1038/sj.eye.6700731.
Kashkouli MB, Jam S, Sabzvari D, Ketabi N, Azarinia S, Seyed Alinaghi S, et al. Thyroid- associated ophthalmopathy in Iranian patients. Acta Medica Iranica. 2011;49(9):612-618.
Carlson SE, Werkman S, Rhodes P, Tolley E. Visual-Acuity Development in Healthy Preterm Infants: Effect of Marine-Oil Supplementation. Am J Clin Nutr. 1993;58(1):35-42. doi: 10.1093/ajcn/58.1.35.
Chandrasekaran S, Petsoglou C, Billson FA, Selva D, Ghabrial R. Refractive change in thyroid eye disease (a neglected clinical sign). Br J Ophthalmol. 2006;90(3):307-309. doi: 10.1136/bjo.2005.078295.
Gürdal C, Saraç O, Genç I, Kırımlıoğlu H, Takmaz T, Can I, et al. Ocular surface and dry eye in graves’ disease. Curr Eye Res. 2011;36(1):8-13. doi: 10.3109/02713683.2010.526285.
Eckstein AK, Finkenrath A, Heiligenhaus A, Renzing-Köhler K, Esser J, Krüger C, et al. Dry eye syndrome in thyroid-associated ophthalmopathy: Lacrimal expression of TSH receptor suggests involvement of TSHRspecific autoantibodies. Acta Ophthalmol Scand 2004;82(3 pt 1):291-297. doi: 10.1111/j.1395-3907.2004.00268.x.
Behrouzi Z, Rabei HM, Azizi F, Daftarian N, Mehrabi Y, Ardeshiri M, et al. Prevalence of open-angle glaucoma, glaucoma suspect, and ocular hypertension in thyroid-related immune orbitopathy. J Glaucoma. 2007;16(4):358-362. doi: 10.1097/IJG.0b013e31802e644b.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.

 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

