External dacryocystorhinostomy for patients of chronic dacryocystitis with chronic rhinosinusitis
Abstract
Introduction: Dacryocystitis is characterized as an inflammatory state of the nasolacrimal sac. It is typically caused by an obstruction within the nasolacrimal duct and subsequent stagnation of tears in the lacrimal sac. Stagnation of tears will provide a favorable environment for infectious organisms to propagate and proteinaceous debris to form.
Materials and Methods: In this prospective, observational study conducted over a 5-year period (March 2011 to February 2016) in a tertiary eye care center and department of Ophthalmology and otorhinolaryngology, consecutive subjects (60 chronic sinusitis patients) were recruited with primary obstruction of the lower lacrimal drainage system due to chronic dacryocystitis who underwent external dacryocystorhinostomy (EDCR) by a single surgeon.
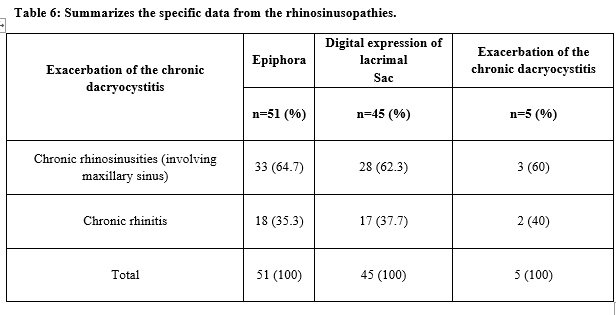
Results: A total of 60 patients were included in this study, concerning the gender, there was a predominance of the female with 39 out of 60 patients (64.1%) and males were 21 patients. Age groups of 1-20 years are 3 patients (4.61%) and predominant age in the study was elderly more than 61 years old patients 40%. The clinical characteristics of chronic dacryocystitis are shown in table 3, epiphora was found in 51 patients (78.4%) and absent in 14 patients (21.5%). The discharge by the digital expression of the lacrimal sac was attained in 45 patients (69.2%) and not attained in 20 patients (30.8%). The previous history of exacerbation of chronic dacryocystitis identified as purulent discharge occurred in 5 patients (7.7%) and non-occurrence in 60 patients (92.3%).
Conclusion: The physiopathology of the CDC is not fully known. This study reveals a possible influence of CRS on the CDC, emphasizing its action on the exacerbation of the symptoms.
Downloads
References
Mauriello JA, Wasserman BA. Acute dacryocystitis: an unusual cause of life-threatening orbital intraconal abscess with frozen globe. Ophthal Plast Reconstr Surg 1996;12(4):294-295.
Cahill KV, Burns JA. Management of acute dacryocystitis in adults. Ophthal Plast Reconstr Surg 1993;9(1):38-41. doi: https://doi.org/10.1097/00002341-199303000-00005.
Barrett RV, Meyer DR. Acquired Lacrimal Fistula Study Group. Acquired lacrimal sac fistula after incision and drainage for dacryocystitis: a multicenter study. Ophthal Plast Reconstr Surg. 2009;25(6):455-457. doi: https://doi.org/10.1097/iop.0b013e3181b80c59.
Yigit O, Samancioglu M, Taskin U, Ceylan S, Eltutar K, Yener M. External and endoscopic dacryocystorhinostomy in chronic dacryocystitis: comparison of results. Eur Arch Otorhinolaryngol. 2007;264(8):879 -885. doi: https://doi.org/10.1007/s00405-007-0286-0.
Chafale VA, Lahoti SA, Pandit A, Gangopadhyay G, Biswas A: Retrobulbar optic neuropathy secondary to isolated sphenoid sinus disease. J Neurosci Rural Pract. 2015;6(2):238-240. doi: https://doi.org/10.4103/0976-3147.153233.
Cyriac JT, Cherian T, Hadi WA, Jose J. Optic neuropathy due to allergic fungal rhinosinusitis. J Neurosci Rural Pract. 2011;2(2):180-182. doi: https://dx.doi.org/10.4103%2F0976-3147.83589.
DeLano MC, Fun FY, Zinreich SJ. Relationship of the optic nerve to the posterior paranasal sinuses: a CT anatomic study. AJNR Am J Neuroradiol. 1996;17(4):669-675.
Munk PL, Lin DT, Morris DC. Epiphora: treatment by means of dacryocystoplasty with balloon dilation of the nasolacrimal drainage apparatus. Radiol. 1990;177(3):687-690. doi: https://doi.org/10.1148/radiology.177.3.2243969.
Heindl LM, Junemann A, Holbach LM. A clinicopathologic study of nasal mucosa in 350 patients with external dacryocystorhinostomy. Orbit. 2009;28(1):7-11. doi: https://doi.org/10.1080/01676830802414806.
DeAngelis D, Hurwitz J, Oestreicher J, Howarth D. The pathogenesis and treatment of lacrimal obstruction: the value of lacrimal sac and bone analysis. Orbit 2001;20(3):163-172. doi: https://doi.org/10.1076/orbi.20.3.163.2626.
Mills DM, Bodman MG, Meyer DR, Morton AD, ASOPRS Dacryocystitis Study Group. The microbiologic spectrum of dacryocystitis: a national study of acute versus chronic infection. Ophthal Plast Reconstr Surg. 2007;23(4):302-306. doi: https://doi.org/10.1097/iop.0b013e318070d237.
Benninger MS, Ferguson BJ, Hadley JA, Hamilos DL, Jacobs M, Kennedy DW et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg 2003; 129(3):S1-32. doi: https://doi.org/10.1016/s0194-5998(03)01397-4.
Hartikainen J, Lehtonen OP, Saari KM. Bacteriology of lacrimal duct obstruction in adults. Br J Ophthalmol. 1997;81:37-40. https://bjo.bmj.com/content/bjophthalmol/81/1/37.full.pdf
Leong SC, Macewen CJ, White PS. A systematic review of outcomes after dacryocystorhinostomy in adults. Am J Rhinol Allergy. 2010;24(1):81-90. doi: https://doi.org/10.2500/ajra.2010.24.3393.
Walland MJ, Rose GE. Factors affecting the success rate of open lacrimal surgery. Br J Ophthalmol 1994;78(12):888-891. doi: https://dx.doi.org/10.1136%2Fbjo.78.12.888.
Fayet B, Racy E, Assouline M. Complications of standardized endonasal dacryocystorhinostomy with unciformectomy. Ophthalmol. 2004;111(4):837-845. doi: https://doi.org/10.1016/j.ophtha.2003.08.023.
Rosenfeld RM, Andes D, Bhattacharyya N, Cheung D, Eisenberg S, Ganiats TG et al. Clinical practice guideline: adult sinusitis. Otolaryngol Head Neck Surg. 2007;137(3):S1-31. doi: https://doi.org/10.1016/j.otohns.2007.06.726.
Dolman PJ. Comparison of external dacryocystorhinostomy with nonlaser endonasal dacryocystorhinostomy. Ophthalmol. 2003;110(1):78-84. doi: https://doi.org/10.1016/s0161-6420(02)01452-5.
Wormald PJ. Powered endoscopic dacryocystorhinostomy. Laryngoscope. 2002;112(1):69-72. doi: https://doi.org/10.1097/00005537-200201000-00013.
Linberg JV, Anderson RL, Bumsted RM, Barreras R. Study of intranasal ostium external dacryocystorhinostomy. Arch Ophthalmol 1982;100(11):1758-1762. doi: https://doi.org/10.1001/archopht.1982.01030040738005.
Warren JF, Seiff SR, Kavanagh MC. Long-term results of external dacryocystorhinostomy. Ophthalmic Surg Lasers Imaging. 2005;36(6):446-450.
Traquair HM. Chronic dacryocystitis. Its causation and treatment. Arch Ophthalmol. 1941;26(165):1. doi: https://dx.doi.org/10.1001/archopht.1941.00870140015001.
Soriano LM, Damasceno NA, Neto GH, Damasceno EF. Comparative study of the clinical profile of chronic dacryocystitis and chronic rhinosinusitis after external dacryocystorhinostomy. Clin Ophthalmol. 2019;13:1267-1271. doi: https://dx.doi.org/10.2147%2FOPTH.S200923.
Madge SN, Chan W, Malhotra R, Ghabrial R, Floreani S, Wormald PJ, et al. Endoscopic dacryocystorhinostomy in acute dacryocystitis: a multicenter case series. Orbit 2011;30(1):1-6. doi: https://doi.org/10.3109/01676830.2010.535952.
Sijuwola OO, Adeyemo AA, Adeosun AA. Orbital complications of rhinosinusitis. Ann Ibadan Postgrad Med. 2007;5(1):6-8.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

