Demographic and clinical profile of venomous snake bite-related ocular manifestations among the paediatric age group in a tertiary care hospital
Abstract
Background: The children having high case fatality and working children (10-14 years) actually belong to the high-risk group of snakebite cases. There is a significant lack of knowledge of the clinical-epidemic profile of snakebite cases in the pediatric age group.
Objectives: To determine the ocular manifestations as well as the magnitude of long-standing visual impairment following snake bite among the pediatric population.
Methods: A prospective observational cross-sectional study was conducted on all the venomous snake bite patients admitted in the pediatric ward of our institution. Bed side ophthalmological evaluation initially by recording visual acuity, ocular position, extraocular movements and anterior segment evaluation were done. Response to treatment and the residual ocular morbidity were also recorded. The collected data were analysed using appropriate statistical methods.
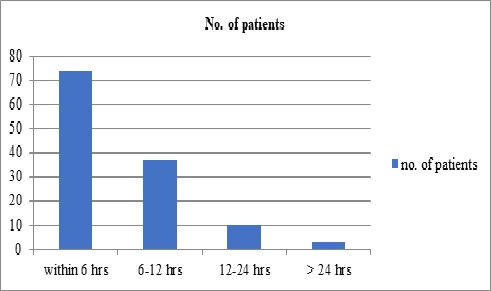
Results: A total of 124 patients were presented to the pediatric department and included in the study. It was observed that males (75.81%) are a more common victim of snakebite whereas lower limb (89.50%) being the common site of snake bite.
Total no of patients: 15 (12.09%) patients had ocular manifestations, dimness of vision is the most common symptom of neurotoxic snake bite followed by ptosis, external ophthalmoplegia, diplopia, optic neuritis, and significant persisting visual impairment. Sub conjunctival hemorrhage (90.90%) being the commonest manifestation of vasculogenic snake bite followed by retinal hemorrhage, vitreous hemorrhage, lid edema, hyphema, anterior uveitis, and significant persisting visual impairment.
Conclusion: Early treatment and close monitoring will help to reduce ocular morbidity. Health education to increase awareness about the hazards of snakebite, early hospital referral, and effective treatment will reduce the global burden of human suffering inflicted by this neglected tropical disease.
Downloads
References
Warrell DA, Gutiérrez JM, Calvete JJ, Williams D. New approaches and technologies of venomics to meet the challenge of human envenoming by snakebites in India. Indian J Med Res. 2013;138(1):38-59.
Prevalence of snakebite envenoming. Available from https://www.who.int/snakebites/epidemiology/en/.
Mohapatra B, Warrell DA, Suraweera W, Bhatia P, Dhingra N, Jotkar RM, et al.; Million Death Study Collaborators. Snakebite mortality in India: A nationally representative mortality survey. PLoS Negl Trop Dis. 2011;5(4):e1018. doi: https://doi.org/10.1371/journal.pntd.0001018.
Hati AK, Mandal M, De MK, Mukherjee H, Hati RN. Epidemiology of snake bite in the district of Burdwan, West Bengal. J Indian Med Assoc. 1992;90(6):145-147.
Bhalla A, Jain AP, Banait S, Jajoo UN, Kalantri SP. Central retinal artery occlusion: an unusual complication of snakebite. J venom Anim Toxins incl Trop Dis. 2004;10(3):311-314. doi: https://doi.org/10.1590/S1678-91992004000300009.
Takeshita T, Yamada K, Hanada M, Oda-Ueda N. Extraocular muscle paresis caused by snakebite. Kobe J Med Sci. 2003;49(1):11-15.
Menon V, Tandon R, Sharma T, Gupta A. Optic neuritis following snake bite. Indian J Ophthalmol. 1997;45(4):236-237. Available from: http://www.ijo.in/text.asp?1997/45/4/236/14993.
Singh J, Singh P, Singh R, Vig VK. Macular infarction following viperine snake bite. Arch Ophthalmol. 2007;125(10):1430-1431. doi: https://doi.org/10.1001/archopht.125.10.1430.
Hayreh SS. Transient central retinal artery occlusion following viperine snake bite. Arch Ophthalmol. 2008;126(6):870-871. doi: https://doi.org/10.1001/archopht.126.6.870-a.
Rao BM. A case of bilateral vitreous haemorrhage following snake bite. Indian J Ophthalmol. 1977;25(2):1-2. Available from: http://www.ijo.in/text.asp?1977/25/2/1/31246.
Iqbal M, Khan BS, Ahmad I. Endogenous Endophthalmitis Associated with Snake Bite. Pak J Ophthalmol. 2009;25(2):114-116.
Law AD, Agrawal AK, Bhalla A. Indian common krait envenomation presenting as coma and hypertension: A case report and literature review. Emerg Trauma Shock. 2014;7(2):126-128. doi: https://doi.org/10.4103/0974-2700.130887.
Patil VC, Patil HV, Patil A, Agrawal V. Clinical Profile and outcome of envenomous snake-bite at tertiary care centre in western Maharashtra. Int J Med Public Health 2011;4(1):28-38. doi: https://doi.org/10.5530/ijmedph.4.2011.7.
Das S, Samadder S, Jana S. Ocular Manifestation and Long-Standing Visual Impairment Following Venomous Snake Bite. J Evolution Med Dent Sci 2015;4(46):7919-7923. doi: https://doi.org/10.14260/jemds/2015/1153.
Tungpakorn N. Unusual visual loss after snakebite. J Venom Toxins Incl Trop Dis. 2010;16(3):519-523. doi: https://doi.org/10.1590/S1678-91992010000300020.
Buttes GP, Ayan N, Cami G. Uveitis after snakebite. Arch Pediatr. 1996;3(8):832-833. doi: https://doi.org/10.1016/0929-693x(96)82175-0.
Kumar PK, Ahuja S, Kumar PS. Bilateral acute anterior uveitis and optic disc edema following a snake bite. Korean J Ophthalmol. 2014;28(2):186-188. doi: https://doi.org/10.3341/kjo.2014.28.2.186.
Nayak SG, Satish R, Nityanandam S, Thomas RK. Uveitis following anti-snake venom therapy. J Venom Toxins Trop Dis. 2007;13(1):13. doi: https://doi.org/10.1590/S1678-91992007000100010.
Seneviratne U, Dissanayake S. Neurological manifestations of snake bite in Sri Lanka. Journal of Postgrad Med. 2002;48(4):275-278. Available from: http://www.jpgmonline.com/text.asp?2002/48/4/275/80.
Singh J, Bhoi S, Gupta V, Goel A. Clinical profile of venomous snake bites in north Indian Military Hospital. J Emerg Trauma Shock. 2008;1(2):78-80. doi: https://doi.org/10.4103/0974-2700.43184.
Bawaskar HS, Bawaskar PH. Envenoming by the common krait (Bungarusbcaeruleus) and Asian cobra (Najanaja): Clinical manifestations and their management in a rural setting. Wilderness Environ Med. 2004;15(4):257-266. doi: https://doi.org/10.1580/1080-6032(2004)015[0257:ebtckb]2.0.co;2.
Lewis RL, Gutmann L. Snake venoms and the neuromuscular junction. Semin Neurol. 2004;24(2):175-179. doi: https://doi.org/10.1055/s-2004-830904.
Kim HD, Jung MS, Kim SY. Exotropia caused by pit viper snakebite. J AAPOS. 2009;13(4):424-425. doi: https://doi.org/10.1016/j.jaapos.2009.04.018.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

