Hyperthyroidism and its association with intraocular pressure and dry eye in teaching medical college
Abstract
Background: Hyperthyroidism associated eye disease is a cosmetically and functionally debilitating disease that is seen worldwide. Objectives: To investigate the association of Hyperthyroidism with Intraocular pressure and Dry eye.
Methods: It was a hospital based cross sectional analysis conducted in teaching medical college for a period of 18 months from January 2018 to July 2019 in hyperthyroid patients, Consecutive sampling was done. Participants were divided into age groups. Hyperthyroidism was clinically and laboratory confirmed. Intraocular pressure and Dry eye were diagnosed by single ophthalmologist. SPSS version 22 was used for analysis. Chi square test was used to determine the association.
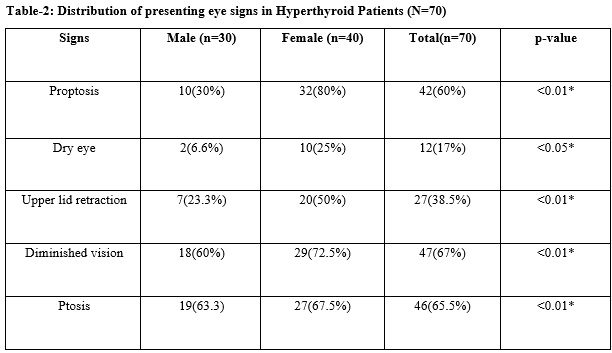
Results: Total 70 established hyperthyroidism patients were studied. The study was female preponderance. Increased Intraocular in hyperthyroid patients was found to be statistically significant. The most common presenting eye sign was found to be diminished vision in almost all patients of Hyperthyroidism which was found to be statistically significant. Age progresses the signs tends to increase in hypothyroidism patients. Diminished vision was found to be the most common eye sign among all age groups which was statistically significant. (p<0.05) followed by Upper lid retraction and ptosis.
Conclusions: Dry eye and increased IOP are commonly seen outcomes that should be managed diligently. This potentially sight- threatening condition is seen worldwide and has many functional and cosmetic consequences that need to be recognized. A larger prospective study will help us to know about the influence of risk factors on the severity of eye problems.
Downloads
References
Wickwar S, McBain HB, Ezra DG, Hirani SP, Rose GE, Newman SP. Which factors are associated with quality of life in patients with Graves’ orbitopathy presenting for orbital decompression surgery? Eye (Land) 2015;29(7):951-957. doi: https://dx.doi.org/10.1038%2Feye.2015.76.
Netland PA, Dallow KL. Thyroid ophthalmopathy. In: Albert DM, Jakobiec FA, editors. Principles and practice of ophthalmology. 3rd ed. Philadelphia: Publisher Elsevier, Saunders 2008; pp: 2937-51.
Wiersinga WM, Bartalena L. Epidemiology and prevention of Graves' ophthalmopathy. Thyroid 2002;12(10): 855-860. doi: https://doi.org/10.1089/105072502761016476.
Rolleston HD. The endocrine organs in health and disease: With an historical review. 1st ed. London: Oxford University Press 1936; pp: 226-227.
Besharati M, Rastegar A. Clinical study of ophthalmopathy in patients with Graves’ disease. Asian J Ophthalmol. 2005;7:108-112.
Tsai CC, Kau HC, Kao SC, Hsu WM. Exophthalmos of patients with Graves' disease in Chinese of Taiwan. Eye (Lond) 2006;20(5):569-573. doi: https://doi.org/10.1038/sj.eye.6701925.
Werner SC. Classification of the eye changes of Graves' disease. Am J Ophthalmol 1969;68(4):646-648. doi: https://doi.org/10.1016/0002-9394(69)91246-x.
Stan MN. Graves' Orbitopathy. 2016 Meet-The- Professor: endocrine case management: the endocrine society 2016; pp: 348-52.
Etezad-Razavi M, Aboutorabi RB, Zarei-Ghanavati S, Daneshvar R. Prevalence and severity of ophthalmic manifestations of Graves' disease in Mashhad university endocrine clinics. Iran J Ophthalmol. 2006;19(3):14-21.
Perros P, Neoh C, Dickinson J. Thyroid eye disease. BMJ 2009;338:b560. doi: https://doi.org/10.1136/bmj.b560.
Kashkouli MB, Jam S, Sabzvari D, Ketabi N, Azarinia S, SeyedAlinaghi S, et al. Thyroid- associated ophthalmopathy in Iranian patients. Acta Medica Iranica. 2011;49(9):612-618.
Lee A, Rochtchina E, Wang J, Healey PR, Mitchell P. Open-angle glaucoma and systemic thyroid disease in an older population. The Blue Mountains Eye Study. Eye (Lond) 2004;18:600-608. doi: https://doi.org/10.1038/sj.eye.6700731.
Haefliger I, von Arx G, Pimentel AR. Pathophysiology of intraocular pressure increase and glaucoma prevalence in thyroid eye disease: a mini-review. Klin Monatsbl Augenheilkund. 2010;227(4):292-293. doi: https://doi.org/10.1055/s-0029-1245199.
Behrouzi Z, Rabei HM, Azizi F, et al. Prevalence of open-angle glaucoma, glaucoma suspect, and ocular hypertension in thyroid-related immune orbitopathy. J Glaucoma. 2007;16(4):358-362. doi: https://doi.org/10.1097/IJG.0b013e31802e644b.
He J, Wu Z, Yan J, Yang H, Mao Y, Ai S, et al. Clinical analysis of 106 cases with elevated intraocular pressure in thyroid-associated ophthalmopathy. Yan Ke Xue Bao. 2004;20(1):10-14.
Eckstein AK, Finkenrath A, Heiligenhaus A, et al. Dry eye syndrome in thyroid‐associated ophthalmo‐pathy: lacrimal expression of TSH receptor suggests involvement of TSHR‐specific autoantibodies. Acta Ophthalmol Scand. 2004;82(3 pt 1):291-297. doi: https://doi.org/10.1111/j.1395-3907.2004.00268.x.
Brabant G, Eckstein A. Management of thyroid eye disease. Endocrine Abstracts 2015;37:MTE4. doi: https://doi.org/10.1530/endoabs.37.MTE4.
Gupta A, Sadeghi PB, Akpek EK. Occult thyroid eye disease in patients presenting with dry eye symptoms. Am J Ophthalmol. 2009;147(5):919-923. doi: https://doi.org/10.1016/j.ajo.2008.12.007.

 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

