A cross sectional study of neutrophil to lymphocyte ratio in patients with benign paroxysmal positional vertigo
Abstract
Background: Benign paroxysmal position vertigo (BPPV) is a disorder which arises due to problem in inner ear. It is the most common cause of vertigo.
Aim: This study evaluates the hs CRP, ESR, NLR, PLR, MHR and bilirubin levels in BPPV patients and compare with levels in healthy subjects.
Materials and Methods: This study is a prospective study which was conducted with 120 newly diagnosed BPPV patients and in 90 patients, age and sex matched.
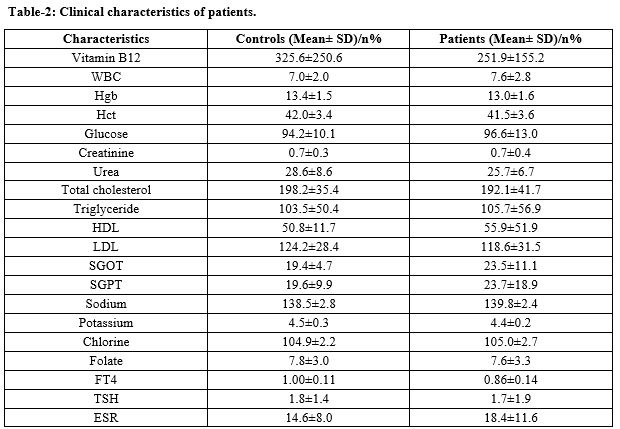
Results: The patients were aged between 15 and 75 years. Females were higher than males in both the groups. Smoking rate was higher in-patient group when compared to the control group. Significant lower levels were observed in BPPV patients for vitamin B12, haematocrit, creatinine, urea, fT4, lymphocyte, total, direct, indirect bilirubin levels. HDL, SGOT, ESR values were significantly higher in BPPV patients. Mean neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR), MPV values were higher significantly in BPPV patients when compared to healthy control patients. Neutrophil, platelet, monocyte, MHR, CRP were almost similar in both the groups.
Conclusion: The potential biomarkers of BPPV were neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR), MPV, erythrocyte sedimentation rate (ESR) and bilirubin levels. The NLR levels were significantly higher in BPPV patients.
Downloads
References
von Brevern M, Bertholon P, Brandt T, Fife T, Imai T, Nuti D, et al. Benign paroxysmal positional vertigo: diagnostic criteria. J Vestib Res. 2015;25(3,4):105-117. doi: https://doi.org/10.3233/VES-150553.
Adam AM. Benign positional vertigo as a clinical manifestation of hyperuricemia - a recent discovery. J Neurol Sci. 2001;187(1):222.
Ziavra NV, Bronstein AM. Is uric acid implicated in benign paroxysmal positional vertigo? J Neurol. 2004;251:115. doi: https://doi.org/10.1007/s00415-004-0277-7.
Jeong SH, Kim JS. The effect of serum uric acid in generating idiopathic benign paroxysmal positional vertigo. Res Vestib Sci. 2010;9(1):27-31.
Hornibrook J. Benign Paroxysmal Positional Vertigo (BPPV): history, pathophysiology, office treatment and future directions. Int J Otolaryngol. 2011:835671. doi: https://doi.org/10.1155/2011/835671.
Tekesin A, Tunc A; Inflammatory biomarkers in benign paroxysmal positional vertigo: A Turkey case-control study. Ideggyógyászati szemle 71(11-12):411-416. doi: https://doi.org/10.18071/isz.71.0411.
Yuan J,Dai J, Li WA, Hu W, Factors associated with benign paroxysmal positional vertigo: A chinese case control study, Med Sci Monit 2017;23:3885-3889. doi: https://doi.org/10.12659/msm.905716.
Yang X, Yang B, Wu M, Wang F, Huang X, Li K, et al. Association between serum uric acid levels and benign paroxysmal positional vertigo: A systematic review and meta-analysis of observational studies; Front. Neurol. 2019;10:91. doi: https://dx.doi.org/10.3389%2Ffneur.2019.00091.
Chen CC, Cho HS, Lee HH, Hu CJ. Efficacy of repositioning therapy in patients with benign paroxysmal positional vertigo and preexisting central neurologic disorders. Front Neurol. 2018;9:486. doi: https://doi.org/10.3389/fneur.2018.00486.
Celikbilek A, Gencer ZK, Saydam L, Zararsiz G, Tanik N, Ozkiris M. Serum uric acid levels correlate with benign paroxysmal positional vertigo. Eur J Neurol. (2014) 21:79-85. doi: https://doi.org/10.1111/ene.12248.
Bhatti I, Peacock O, Lloyd G, Larvin M, Hall RI. Preoperative hematologic markers as independent predictors of prognosis in resected pancreatic ductal adenocarcinoma: neutrophil-lymphocyte versus platelet-lymphocyte ratio.. Am J Surg. 2010;200(2):197-203. doi: https://doi.org/10.1016/j.amjsurg.2009.08.041.
He W, Yin C, Guo G, Jiang C, Wang F, Qiu H, et al. Initial neutrophil lymphocyte ratio is superior to platelet lymphocyte ratio as an adverse prognostic and predictive factor in metastatic colorectal cancer. Med Oncol. 2013;30(1):439. doi: https://doi.org/10.1007/s12032-012-0439-x.
Mano Y, Shirabe K, Yamashita Y, et al Preoperative neutrophil-to-lymphocyte ratio is a predictor of survival after hepatectomy for hepatocellular carcinoma: a retrospective analysis.. Ann Surg. 2013;258(2):301–305. doi: https://doi.org/10.1097/SLA.0b013e318297ad6b.
Yucel C, Keskin MZ, Cakmak O, Ergani B1, Kose C2, Celik O, et al Predictive value of pre-operative inflammation-based prognostic scores (neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and monocyte-to-eosinophil ratio) in testicular sperm extraction: a pilot study.. Androl. 2017;5(6):1100–1104. doi: https://doi.org/10.1111/andr.12417.
Liu CL, Lee JJ, Liu TP, Chang YC, Hsu YC, Cheng SP. Blood neutrophil-to-lymphocyte ratio correlates with tumor size in patients with differentiated thyroid cancer. J Surg Oncol. 2013;107(5):493-497. doi: https://doi.org/10.1002/jso.23270.
Gooden MJ, De Bock GH, Leffers N, Daemen T, Nijman HW. The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with meta-analysis. Br J Cancer. 2011;105(1):93-103. doi: https://doi.org/10.1038/bjc.2011.189.
Motomura T, Shirabe K, Mano Y, Muto J, Toshima T, Umemoto Y, et al. Neutrophil-lymphocyte ratio reflects hepatocellular carcinoma recurrence after liver transplantation via inflammatory microenvironment. J Hepatol. 2013;58(1):58-64. doi: https://doi.org/10.1016/j.jhep.2012.08.017. Epub 2012 Aug 25.
Yu YJ, Li N, Yun ZY, Niu Y, Xu JJ, Liu ZP, et al Preoperative mean platelet volume and platelet distribution associated with thyroid cancer. Neoplasma. 2017;64(4):594-598. doi: https://doi.org/10.4149/neo_2017_414.

 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

