Orbital cysticercosis: varied presentations with management plan
Abstract
Introduction: Cysticercosis is a systemic parasitic disease caused by the larval form of the cestode pork tapeworm, Taenia solium. Along with subcutaneous tissue and skeletal muscles, eyes, brain, bladder wall, and heart are also the commonly involved sites of lodgment of the larva. The larval lodgment at these sites causes potentially harmful and variable clinical manifestations. Ocular cysticercosis can be extraocular or intraocular.
Material and Methods: An immunologic reaction with fairly intense inflammatory signs and symptoms may be produced, and the surrounding structures may be compressed. Acquired strabismus, diplopia, recurrent redness, and painful proptosis are some of the clinical signs in patients with orbital cysticercosis. The present study report 8 cases of ocular cysticercosis with a variety of clinical presentations depending on the exact site of larval involvement.
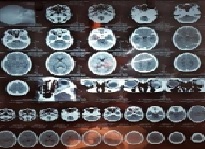
Result: Patient CT Scan was done to confirm the clinical diagnosis in most of the posterior segment and orbital lesions. Rest investigations were within normal limits.
Conclusions: It becomes important to report these cases because of the relative rarity of the condition these days, myriads of presentation and age group, the relative concentration of cases in endemic areas, and CT Scan used as the definitive investigation to confirm orbital cysticercosis and rule out neurocysticercosis.
Downloads
References
Daniel Albert, Frederick Jakobiec, Nancy Robinson.Principles& Practice of Ophthalmology, W.B. Saunders Co, copyright 1994;462,1711–1751,2308,2319,3073.
Ryan SJ. Ocular Cysticercosis Retina. 2nd ed. vol. 2. St. Louis (USA): C. Mosby and Co; 1994.
Malik SRK, Gupta AK, Chowdhary S. Ocular Cysticercosis. Am J Ophthalmol. 1986; 66:1168-1171.
Rath S, Honavar SG, Naik M, Anand R, Agarwal B, Krishnaiah S, et al. Orbitalcysticercosis: clinical manifestations, diagnosis, management,and outcome. Ophthalmol. 2010;117(3):600-605. doi: https://doi.org/10.1016/j.ophtha.2009.07.030.
Pushker N, Bajaj MS, Chandra M. Ocular and orbital cysticercosis. Acta Ophthalmol Scand. 2001;79(4):408-413. doi: https://doi.org/10.1034/j.1600-0420.2001.079004408.x.
Reddy PS, Satyendran OM. Ocular cysticercosis. Am. J.Ophthalmol. 1964;57:664-666.
Sen DK, Mathur RN, Thomas A. Ocular cysticercosis in India. Br J Ophthalmol. 1967;51(9):630-632. doi: https://doi.org/10.1136/bjo.51.9.630.
Bodh SA, Kamal S, Kumar S, Goel R, Nagpal S, Aditya K. Orbital Cysticercosis. Del J Ophthalmol. 2012;23(2):99-103. doi: http://dx.doi.org/10.7869/djo.2012.50.
Sundaram PM, Jayakumar N, Noronha V. Extraocular musclecysticercosis – a clinical challenge to the ophthalmologists. Orbit. 2004;23(4):255-262. doi: https://doi.org/10.1080/01676830590889866.
Verma R, Jaiswal A. Multiple brain parenchymal neurocysticercosis with extraocular muscle cysticercosis affecting levator palpebralsuperioris and superior rectus complex: an unusual association. BMJ Case Rep. 2013;25. doi: http://dx.doi.org/10.1136/bcr-2012-007421.
Goyal S, Sandhu PS, Sharma A, Malik MA, Bansal P, Kaur J. Inferior rectus muscle ocular cysticercosis: A case report. Saudi J Ophthalmol. 2015;29(2):175-177. doi: https://doi.org/10.1016/j.sjopt.2014.11.002.
Pushker N, Mehta M, Meel R, Bajaj MS. Disseminated cysticercosis with multiple bilateral orbital cysts. Ophthal Plast Reconstr Surg. 2009;25(6):499-501. doi: https://doi.org/10.1097/iop.0b013e3181b82085.
Topilow HW, Yimoyines DJ, Freeman HM, Young GA, Addison R, et al. Bilateral multifocal intraocular cysticercosis. Ophthalmol. 1981;88(11):1166-1172. doi: https://doi.org/10.1016/s0161-6420(81)34890-8.
Sekhar GC, Honavar SG. Myocysticercosis: Experience with imaging and therapy. Ophthalmol. 1999;106(12):2336-2340. doi: https://doi.org/10.1016/s0161-6420(99)90537-7.
Bansal RK, Gupta A, Grewal SP, Mohan K. Spontaneous extrusion of cysticercosis: report of three cases. Ind. J Ophthalmol. 1992;40(2):59-60. Available from: http://www.ijo.in/text.asp?1992/40/2/59/24401.
Goyal JL, Das S, Kumar S, Chauhan D, Baheti U, Sangit V. Retrobulbar Cysticercosis Masquerading asOptic Nerve Glioma. Orbit. 2007;26(1):61-63. https://doi.org/10.1080/01676830600675046.
Honavar SG, Sekhar CG. Ultrasonological characteristics of extraocular cysticercosis. Orbit. 1998;17(4):271- 284. doi: https://doi.org/10.1076/orbi.17.4.271.2739.
Murthy GR, Rao AV. Sub-conjunctival cysticercosis. Indian J Ophthalmol. 1980;28(2):77-78. Available from: http://www.ijo.in/text.asp?1980/28/2/77/28228.
Kaur A, Agrawal A, Agrawal PK, Goel MM. Lacrimal canalicular obstruction by cysticercus cellulosae. Orbit. 2006;25(2):163-165. doi: https://doi.org/10.1080/01676830600666193.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

