Effect of donor and host factors on corneal graft transparency
Jain A.1*, Joshi H.2, Jain N.3
DOI: https://doi.org/10.17511/jooo.2021.i04.01
1* Amisha Jain, Assistant Professor, Department of ophthalmology, S.B.KS. M.I and R.C., Dhiraj General Hospital, Piparia, Gujrat, India.
2 Hema Joshi, Cataract, Cornea and Ocular surface, H V Desai Eye Hospital, Pune, Maharashtra, India.
3 Nimish Jain, Assistant Professor, Department of Cardiac Anaesthesia, S.B.KS. M.I and R.C., Dhiraj General Hospital, Piparia, Gujrat, India.
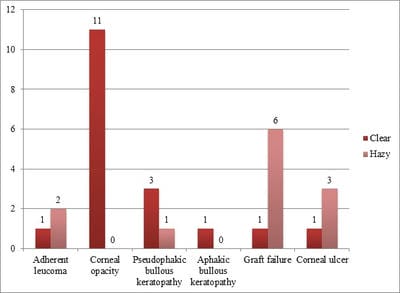
Objective: To study the correlation between donor factors and recipients' factors on graft clarity. Materials and methods: The study comprised 30 cases of Keratoplasty surgery with a follow up of 6 months. All donor corneas were evaluated by Konan specular microscope for endothelial cell count; details of the donor like age, cause of death were noted. The patients were divided into two groups, Group 1 had graft failure, and Group 2 had clear corneas. Observation and Result: There were 12 patients in group 1 and 18 patients in group 2 with six months of follow up. The mean endothelial cell count in group 1 was 1942.3/mm2, and group 2 was 2334.8/mm2. There is a significant difference in the mean endothelial cell count between the two groups. On analysing the indication for Keratoplasty in two groups, the outcome was best for the corneal opacity group during worst for the graft failure group. Conclusion: Donor endothelial cell count significantly influenced graft outcome; rest donor factors (age, death enucleation interval, enucleation surgery interval) don't affect graft survival. Indication for Keratoplasty is a significant predictor of graft survival.
Keywords: Donor factors, Endothelial cell count, Keratoplasty, Graft failure, Indication for Keratoplasty, Host factors
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of ophthalmology, S.B.KS. M.I and R.C., Dhiraj General Hospital, Piparia, Madhya Pradesh, India. Email: |
Jain A, Joshi H, Jain N. Effect of donor and host factors on corneal graft transparency. Trop J Ophthalmol Otolaryngol. 2021;6(4):56-61. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/206 |


 ©
©