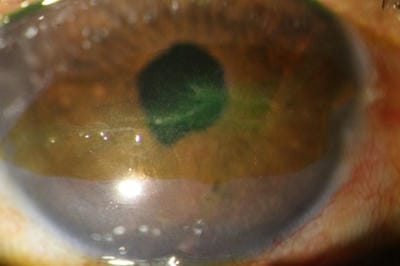
Brown’y points for guessing!- A case report of an unusual pigmented corneal plaque.
Joshi H.1, Bobade Veer A.2*, Joshi S.3, Deshpande M.4
DOI: https://doi.org/10.17511/jooo.2021.i03.02
1 Hema Joshi, (MBBS, DOMS, DNB), Department of Cornea, PBMA’s H V Desai Eye Hospital, Pune, Maharashtra, India.
2* Amrapali Bobade Veer, (MBBS, DOMS, DNB), Department of Cornea, PBMA’s H V Desai Eye Hospital, Pune, Maharashtra, India.
3 Shilpa Joshi, (MBBS, DOMS, FICO), Department of Cornea, PBMA’s H V Desai Eye Hospital, Pune, Maharashtra, India.
4 Madan Deshpande, (Retd) Col, (MBBS, MS), Department of Cornea, PBMA’s H V Desai Eye Hospital, Pune, Maharashtra, India.
A 54-year-old female presented with complaints of blurring in the right eye since 2 years. A grade 3 nuclear sclerosis and a peculiar band-shaped subepithelial brown corneal patch, within the inter-palpebral area was noted. The overlying epithelium was scraped for smears and cultures which came back negative. The patient underwent uneventful cataract surgery, but returned 2 weeks later with complaints of watering and grittiness. Surprisingly a dendritic ulcer was noted within the pigmented patch, which responded to topical antivirals and tear substitutes. History of a similar episode, 3 years back was elicited upon questioning the patient.
Keywords: HSV keratitis, Corneal pigmentation, Subepithelial plaque
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , (MBBS, DOMS, DNB), Department of Cornea, PBMA’s H V Desai Eye Hospital, Pune, Maharashtra, India. Email: |
Joshi H, Veer AB, Joshi S, Deshpande M. Brown’y points for guessing!- A case report of an unusual pigmented corneal plaque.. Trop J Ophthalmol Otolaryngol. 2021;6(3):46-49. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/200 |


 ©
©