Ocular Manifestations Of Carotid Cavernous Fistula and Clinical Outcome After Management
Gantela S.1*, Chowdary N.2, M. S.3
DOI: https://doi.org/10.17511/jooo.2021.i03.01
1* Sirisha Gantela, MS Ophthalmology Professor, Department of Ophthalmology, NRI Medical College and General Hospital, Guntur, Andhra Pradesh, India.
2 N. Lakshmi Chowdary, MS Ophthalmology Professor, Department of Ophthalmology, NRI Medical College and General Hospital, Guntur, Andhra Pradesh, India.
3 Satyanarayana M., MD DM Neuroradiology Interventional radiologist Associate professor, Department of Radiology, NRI Medical College and General Hospital, Guntur, Andhra Pradesh, India.
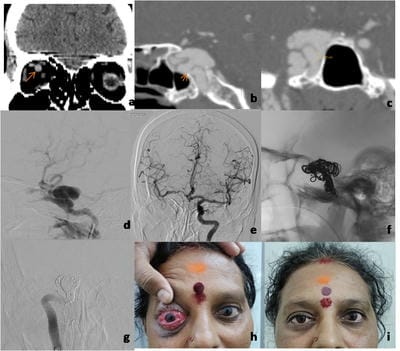
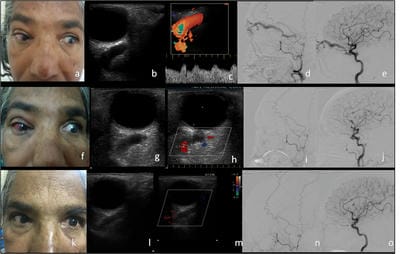
Aim: The purpose of the study is to report the ocular manifestations of Carotid cavernous fistula. To confirm the diagnosis by radiological investigations and to evaluate the clinical outcome after management. Materials and Methods: Patients who presented to the ophthalmology department with signs and symptoms of carotid-cavernous fistula were evaluated by clinical examination followed by radiological investigations like ultrasound, Doppler, CT scan and MRI. They later underwent DSA ( Digital Subtraction Angiography) for confirmation followed by definitive treatment. Results: Out of four patients who had direct CCF, three cases were managed by endovascular embolization of the parent artery. The remaining one case was conservatively managed by carotid massage as it was a low flow fistula and the patient also had Parkinson’s disease. Four cases that had indirect CCF were managed by carotid massage. Complete closure of the fistula is seen in all cases. Patients were followed up for 1 month, 3 months and 6 months and clinical outcome was evaluated. Conclusion: CCF should be suspected in the presence of arteriolised conjunctival vessels, proptosis and audible bruit. Diagnosis is by radiological tests like ultrasonography, Doppler, CT scan and MRI. The confirmatory test is digital subtraction angiography (DSA). Direct CCF is effectively treated with endovascular therapy by coiling the fistula and indirect CCF is managed by manual compression. Early diagnosis and treatment can prevent sight-threatening complications.
Keywords: Carotid Cavernous Fistula, Digital Subtraction Angiography, Endovascular management, Manual Carotid Compression, Proptosis
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , MS Ophthalmology Professor, Department of Ophthalmology, NRI Medical College and General Hospital, Guntur, Andhra Pradesh, India. Email: |
Gantela S, Chowdary NL, Satyanarayana M. Ocular Manifestations Of Carotid Cavernous Fistula and Clinical Outcome After Management. Trop J Ophthalmol Otolaryngol. 2021;6(3):40-45. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/199 |


 ©
©