Incidence, management, and outcome of complex cataracts in a tertiary eye set up
Verma R.1, Shrishrimal M.2, Gokharu S.3, Shah D.4*
DOI: https://doi.org/10.17511/jooo.2020.i08.02
1 Ritu Verma, Cornea and Cataract Consultant, Department of Ophthalmology, Choithram Netralaya, Shriram Talawali, Indore, Madhya Pradesh, India.
2 Meghna Shrishrimal, Senior Resident, Department of Ophthalmology, Choithram Netralaya, Shriram Talawali, Indore, Madhya Pradesh, India.
3 Shirali Gokharu, DNB Resident, Department of Ophthalmology, Choithram Netralaya, Shriram Talawali, Indore, Madhya Pradesh, India.
4* Dhaivat Shah, Vitreoretina Consultant, Department of Ophthalmology, Choithram Netralaya, Shriram Talawali, Indore, Madhya Pradesh, India.
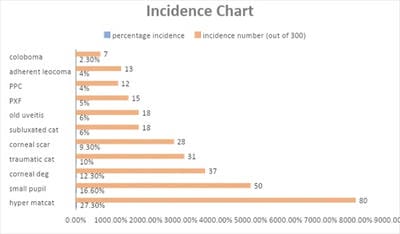
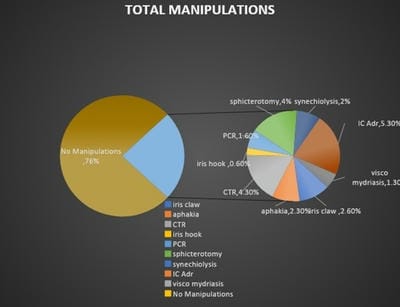
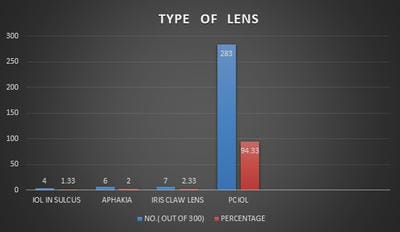
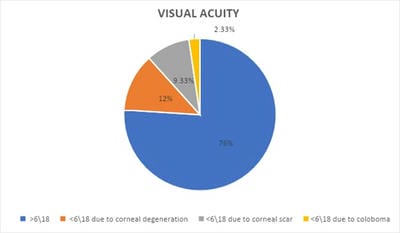
Aim: To study the incidence, management, and outcome of complex cataract cases in a tertiary eye care center. Material and methods: Retrospective observational study with analysis of records done for patients who were operated on for complex cataract from December 2019 to February 2020. Results: 300/10,000 patients had complex cataracts requiring additional surgical skills, advanced equipment, and better patient counseling. 5.3% (16/300) of patients needed intracameral adrenaline whereas 1.3% (4/300) needed Visco mydriasis. A capsular tension ring was implanted in 4.3%(13/300) of patients. 4% (12/300) underwent sphincterotomies whereas 2% (6/300) had to undergo synechiolysis. Iris hooks were used in only 0.6% of patients (2/300). Posterior capsular rent was seen in 1.6%(5/300) which was managed by placing a Posterior chamber IOL in the sulcus. 2.6% (8/300) had implantation of the iris-claw lens and 2.3% (7/300) were left aphakic for secondary IOL to be implanted at a later date. The visual outcome was better than 6/18 in 76% of patients. 24% of patients had an improvement in their visual acuity by a line or 2 but was less than 6/18 due to corneal degenerations, corneal scarring, Retinal pathologies, and colobomas. Conclusion: Although these cataracts demand more expertise on behalf of the surgeon, the outcome can be very rewarding if done with proper planning. The knowledge of small incision cataract surgery is highly valuable in such situations.
Keywords: Complex cataracts, Intraoperative Manipulations, Visual outcome
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Vitreoretina Consultant, Department of Ophthalmology, Choithram Netralaya, Shriram Talawali, Indore, Madhya Pradesh, India. Email: |
Verma R, Shrishrimal M, Gokharu S, Shah D. Incidence, management, and outcome of complex cataracts in a tertiary eye set up. Trop J Ophthalmol Otolaryngol. 2020;5(8):207-215. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/174 |


 ©
©