Change to win - flapless external dacryocystorhinostomy (DCR)
Ranjan R.1*, Rupam K.2, Kumar S.3
DOI: https://doi.org/10.17511/jooo.2020.i08.04
1* Ravi Ranjan, Awadh Medicare, Bikramganj, Bihar, India.
2 Kumari Rupam, Consultant, Awadh Medicare, Bikramganj, Bihar, India.
3 Sudhir Kumar, Associate Professor, Government Medical College, Bettiah, Bihar, India.
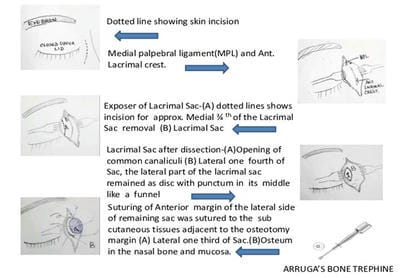
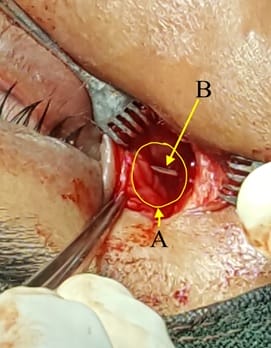
Introduction: Nasolacrimal Duct obstruction (NLDO) is a common ophthalmic problem and the usual Treatment is Dacryocystorhinostomy (DCR), either external or endonasal. This study aims to evaluate the success of external DCR with neither anterior nor posterior flaps with Mitomycin c (MMC) syringing on the 5th post-operative day (early proliferative phase of wound healing). It was shown in the present study that a comparable good result can be achieved without tedious flaps making and anastomosis. Material and Methods: It is a retrospective, non-comparative observational Case series study done from March 2011 to August 2019. A total of 2165 patients were included in this study qualifying inclusion criterion. 8 to 10 mm Arruga’s bone trephine was used to make osteum in lacrimal bone and passage in the nasal mucosa. The anterior margin of the lateral side of the remaining sac was sutured to the subcutaneous tissue of the medial side adjacent to the nasal osteotomy. Syringing with 1 ml of 0.4 mg/ ml MMC was done in the newly formed passage on the 5th post-operative day. These patients were followed up for one year. The success criteria were symptomatic relief from epiphora subjectively. Objectively a patent nasolacrimal duct upon syringing and Nasal endoscopy. Results: 2136 (out of 2165) patients' eyes treated with this procedure showed resolution of epiphora with a success rate of 98.66%. Conclusion: The current study suggest that DCR without flap making is an effective and easy procedure in the management of NLDO obstruction and flap making is a futile step in the procedure as it has no impact on the outcome.
Keywords: Nasolacrimal Duct obstruction (NLDO), Flapless external Dacryocystorhinostomy(DCR), Arruga’s bone trephine, Mitomycin c syringing
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Awadh Medicare, Bikramganj, Bihar, India. Email: |
Ranjan R, Rupam K, Kumar S. Change to win - flapless external dacryocystorhinostomy (DCR). Trop J Ophthalmol Otolaryngol. 2020;5(8):224-230. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/169 |


 ©
©