Awareness and knowledge of ocular prophylactic measures and hand hygiene among medical students in the wake of the pandemic- COVID 19
Varsha V.1, Ramachandra S.2*
DOI: https://doi.org/10.17511/jooo.2020.i06.04
1 Varsha V., Third Year Post-Graduate, Department of Ophthalmology, Sri Devaraj Urs Medical College, Kolar, Karnataka, India.
2* Sandhya Ramachandra, Professor and Head of Department, Department of Ophthalmology, Sri Devaraj Urs Medical College, Kolar, Karnataka, India.
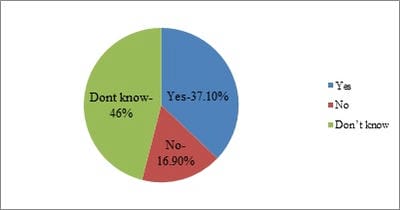
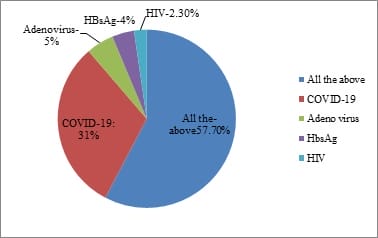
Objective: To assesses the awareness and knowledge of ocular prophylaxis, hand hygiene, and ocular surface as a mode of spread of SARS-CoV-2 among medical students, in the wake of the pandemic COVID-19. Methods: A cross-sectional questionnaire-based study was conducted on 248 medical students. The questionnaire is constructed based on previous publications related to hand hygiene and ocular hygiene. The answers to all the questions were assessed and results were analyzed. Results: Out of the 248 people who were included in the study, 99.2% were aware of the importance of handwashing and 97.6% of them agreed that handwashing is required after examining every patient. 85.5% of the participants agreed that the ophthalmologist needs to wear N95 masks during the slit-lamp examination and 92.9% of the students were aware of the need for protective eye goggles. 85.9% agreed that the patients also need to wear protective masks while being examined.74.3% of the participants knew the moments of handwashing, 60.2% knew the correct number of steps of handwashing. 87.6% answered that the slit lamp should be cleaned after every patient. Only 36.5% of the students who participated knew that non-contact tonometry will produce aerosols. The Internet was the most important source of information in about 27% of the participants. Conclusion: Medical students’ knowledge about COVID-19 and the prophylactic measures needs reinforcement. This is essential to safeguard the health of the medical professionals against less understood and remote routes of viral spread.
Keywords: COVID-19, Ocular prophylaxis, Hand hygiene, Medical students, Awareness, Knowledge
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor and Head of Department, Department of Ophthalmology, Sri Devaraj Urs Medical College, Kolar, Karnataka, India. Email: |
Varsha V, Ramachandra S. Awareness and knowledge of ocular prophylactic measures and hand hygiene among medical students in the wake of the pandemic- COVID 19. Trop J Ophthalmol Otolaryngol. 2020;5(6):138-143. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/154 |


 ©
©