A case report: bilateral choanal atresia in a nine-year-old female child
Shaik W.1*, Aradhyula D.2, Rao Yedluri S.3
DOI: https://doi.org/10.17511/jooo .2020.i06.09
1* Wahid Shaik, Senior Resident, Department Of Otorhinolaryngology, NRI Academy of Sciences, Guntur, Andhra Pradesh, India.
2 Dinesh Aradhyula, Post-Graduate, Department Of Otorhinolaryngology, NRI Academy of Sciences, Guntur, Andhra Pradesh, India.
3 Satya Prabhakar Rao Yedluri, Professor and Head of The Department, Department Of Otorhinolaryngology, NRI Academy of Sciences, Guntur, Andhra Pradesh, India.
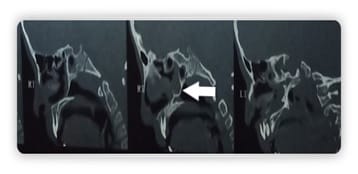
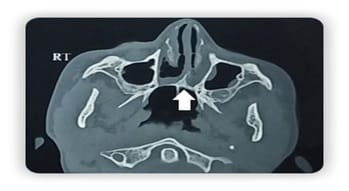
Choanal atresia is a rare congenital malformation of the nasal cavity characterized by obliteration of posterior choanae. It can be unilateral or bilateral. Bilateral choanal atresia is one of the life-threatening conditions and survival up to adulthood is rare A 9-year-old female presented to our department with complaints of a bilateral nasal block, nasal discharge, snoring, anosmia, and mouth breathing. Diagnostic nasal endoscopy and computerized tomography of the nose and paranasal sinuses revealed bilateral choanal atresia. Transnasal endoscopic choanoplasty was performed and discharged on postoperative day 7. Postoperative follow up on two weeks showed significant improvement in symptoms and endoscopy revealed bilateral patent posterior choanae. The child with bilateral choanal atresia surviving up to nine years of age is rare. In contrast to unilateral choanal atresia, bilateral choanal atresia is a diagnostic and therapeutic emergency. Diagnostic nasal endoscopy and computerized tomography help in planning surgery. Minimally invasive endoscopic choanoplasty has replaced the transpalatal approach.
Keywords: Choanal atresia, Congenital, Choanoplasty
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Senior Resident, Department Of Otorhinolaryngology, NRI Academy of Sciences, Guntur, Andhra Pradesh, India. Email: |
Shaik W, Aradhyula D, Yedluri S R P. A case report: bilateral choanal atresia in a nine-year-old female child. Trop J Ophthalmol Otolaryngol. 2020;5(6):168-171. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/150 |


 ©
©