Comparison of conjunctival free autograft and Rotational flap technique in primary pterygium surgery: Visual changes and safety profiles
Chaurasia P.1, Chaurasia V.2*
DOI: https://doi.org/10.17511/jooo.2021.i03.03
1 Pawan Chaurasia, Assistant Professor, Department of Opthalmology, Peoples College of medical sciences, Bhopal, Madhya Pradesh, India.
2* Vaishali Chaurasia, Associate Professor, Department of Obstetrics and Gynecology, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
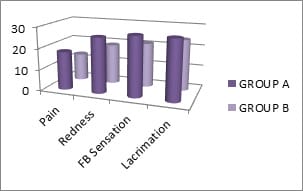
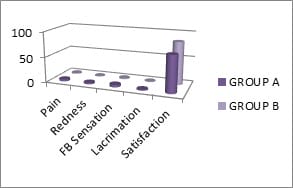
Aims and objectives: To evaluate the postoperative symptomatic comfort, visual changes, complication and rate of recurrence in free conjunctival autograft and rotational flap technique in primary pterygium surgery. Materials & Methods: This prospective study was conducted in 60 eyes of 60 patients, presented with primary progressive nasal pterygium larger than 1mm causing symptomatic discomfort, astigmatism and cosmetic disfigurement. Patients were divided into two groups randomly. In group A, patients with pterygium excision with free conjunctival autograft and group B, pterygium excision with rotation flap technique were included. Post-operative day 1 symptomatic comfort (symptoms and signs), graft stability, corneal clarity and any complication were noted. Visual acuity (VA), auto-refracto keratometer measurements and detailed biomicroscopic examinations, were performed preoperatively and postoperatively at 1month and 3 months. Results: Most of the patients in our study were in the middle age group of 40-49 years (41.6%). Out of 60 patients, 35 were males (58.4%) and 25 were females (41.6%). Patients with outdoor activities had a higher prevalence of pterygium (78.4%). The incidence of pterygium was more in the right eye (60%) than left eye (40%). Of the 60 patients, Grade I, II and III pterygium was 20%, 56.7% and 23.3% in group A and 16.7%, 63.3% and 20% in group B respectively. The mean symptomatic score was statistically significantly higher for group A for each factor (P<0.05). In the 3rd month, the overall patient’s satisfaction score was significantly higher in group B (P<0.05). Conclusion: Both surgical techniques were equally effective in terms of visual acuity, astigmatism and recurrence. The patient’s satisfaction score was significantly higher in the rotation flap technique group.
Keywords: Pterygium, Conjunctival free autograft, Rotational flap
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Obstetrics and Gynecology, Gandhi Medical College, Bhopal, Madhya Pradesh, India. Email: |
Chaurasia P, Chaurasia V. Comparison of conjunctival free autograft and Rotational flap technique in primary pterygium surgery: Visual changes and safety profiles. Trop J Ophthalmol Otolaryngol. 2021;6(3):50-55. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/149 |


 ©
©