Effectiveness of Low Vision Aids in patients with low vision attending a medical college hospital
Abdul Aziz A.1, Kulkarni U.2*
DOI: https://doi.org/10.17511/jooo.2020.i04.02
1 Almas Abdul Aziz, Assistant Professor, College of Optometry, Al Salama Eye Hospital, Malappuram, Kerala, India.
2* Uma Kulkarni, Professor, Department of Ophthalmology, Yenepoya Medical College, Mangalore, Karnataka, India.
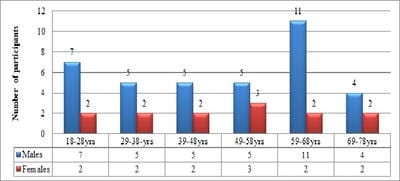
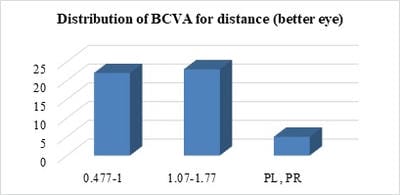
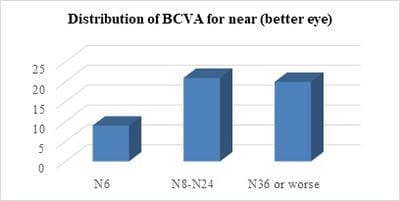
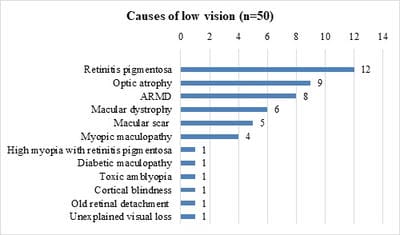
Introduction:Low vision is defined as visual impairment despite treatment, surgery, or standard refractive correction, but with the potential to use the residual vision. The aim of the study was to explore the clinical profile of patients requiring Low Vision Aids (LVA) and assess the effectiveness, of LVA among patients with low vision. Material and Methods: Fifty patients fulfilling the criteria of low vision were recruited after obtaining informed written consent and detailed ocular evaluation was done to detect the cause of low vision. A trial of LVAs was done for near using hand-held magnifiers (+6D, +14D, +20D), stand magnifiers (+8D, +14D, +20D) and spectacle magnifiers (+6D, +10D, +14D, +20D) and visual improvement was noted. Similarly, LVAs were tried for distance using telescope 2.5X and clip-on telescope 3X. Results: The majority of the participants (72%) belonged to the upper lower class. The most common causes of low vision were heritable conditions like retinitis pigmentosa (24%), bilateral primary optic atrophy (18%), and macular dystrophies (16%). The most effective low vision aids were handheld and stand magnifiers which improved vision by one to four lines. The magnifiers were most effective in eyes with macular dystrophy, retinitis pigmentosa, and age-related macular degeneration. Conclusion:Low vision aids are potential methods of improving the residual vision in low vision patients. In the background of the high and increasing prevalence of low vision and poor awareness about low vision aids among them, efforts are necessary to rehabilitate them with affordable and accessible low vision services.
Keywords: Low vision, Residual vision, Low Vision Aids, Handheld and stand magnifiers, Telescopes
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor, Department of Ophthalmology, Yenepoya Medical College, Mangalore, Karnataka, India. Email: |
Aziz AA, Kulkarni U. Effectiveness of Low Vision Aids in patients with low vision attending a medical college hospital. Trop J Ophthalmol Otolaryngol. 2020;5(4):88-95. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/137 |


 ©
©