Demographic and clinical profile of venomous snake bite-related ocular manifestations among the paediatric age group in a tertiary care hospital
Jana S.1, Ray S.2*, Banerjee M.3
DOI: https://doi.org/10.17511/jooo.2020.i03.04
1 Subhasis Jana, Senior Resident, Department of Ophthalmology, Burdwan Medical College and Hospital, Burdwan, West Bengal, India.
2* Soumya Ray, M.B.B.S., M.S.(PGT), Junior Resident, Department of Ophthalmology, Burdwan Medical College and Hospital, Burdwan, West Bengal, India.
3 Mousumi Banerjee, Head of the Department, Department of Ophthalmology, Burdwan Medical College and Hospital, Burdwan, West Bengal, India.
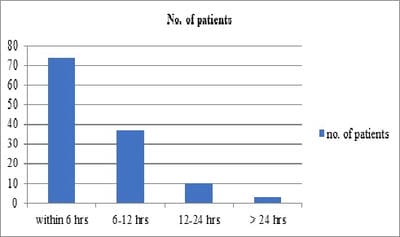
Background: The children having high case fatality and working children (10-14 years) actually belong to the high-risk group of snakebite cases. There is a significant lack of knowledge of the clinical-epidemic profile of snakebite cases in the pediatric age group. Objectives: To determine the ocular manifestations as well as the magnitude of long-standing visual impairment following snake bite among the pediatric population. Methods: A prospective observational cross-sectional study was conducted on all the venomous snake bite patients admitted in the pediatric ward of our institution. Bed side ophthalmological evaluation initially by recording visual acuity, ocular position, extraocular movements and anterior segment evaluation were done. Response to treatment and the residual ocular morbidity were also recorded. The collected data were analysed using appropriate statistical methods. Results: A total of 124 patients were presented to the pediatric department and included in the study. It was observed that males (75.81%) are a more common victim of snakebite whereas lower limb (89.50%) being the common site of snake bite. Total no of patients: 15 (12.09%) patients had ocular manifestations, dimness of vision is the most common symptom of neurotoxic snake bite followed by ptosis, external ophthalmoplegia, diplopia, optic neuritis, and significant persisting visual impairment. Conclusion: Early treatment and close monitoring will help to reduce ocular morbidity. Health education to increase awareness about the hazards of snakebite, early hospital referral, and effective treatment will reduce the global burden of human suffering inflicted by this neglected tropical disease.
Keywords: Venomous snake bite, Ocular manifestations, Ocular morbidity
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , M.B.B.S., M.S.(PGT), Junior Resident, Department of Ophthalmology, Burdwan Medical College and Hospital, Burdwan, West Bengal, India. Email: |
Jana S, Ray S, Banerjee M. Demographic and clinical profile of venomous snake bite-related ocular manifestations among the paediatric age group in a tertiary care hospital. Trop J Ophthalmol Otolaryngol. 2020;5(3):78-83. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/136 |


 ©
©