A case report of oculofacial rosacea complicating to corneal infiltrates and vascularisation
Chanekar S.1*, P. S. Usgaonkar U.2, O Akarkar S.3
DOI: https://doi.org/10.17511/jooo.2020.i02.04
1* Samruddhi Chanekar, Junior Resident, Department of Ophthalmology, Goa Medical College, Bambolim, Goa, India.
2 Ugam P. S. Usgaonkar, Professor and Head, Department of Ophthalmology, Goa Medical College, Bambolim, Goa, India.
3 Shekhar O Akarkar, Senior Resident, Department of Ophthalmology, Goa Medical College, Bambolim, Goa, India.
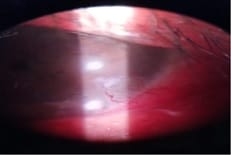
Purpose: To report a case of ocular rosacea with corneal infiltrates and vascularisation. Here we report a case of a 34-year-old male presenting with ocular rosacea with corneal infiltrates and vascularisation in the left eye with posterior blepharitis of both eyes. The clinical diagnosis was based on the facial findings of erythematous papulomacular lesions and telangiectasia. The patient was treated with systemic doxycycline and for ocular lesions treated with antibiotic steroids and lubricants. Ocular rosacea, if not treated on time, can worsen to the stage of corneal infiltrates and vascularisation.
Keywords: Ocular rosacea, Corneal infiltrates, Blepharitis
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Junior Resident, Department of Ophthalmology, Goa Medical College, Bambolim, Goa, India. Email: |
Chanekar S, Usgaonkar UPS, Akarkar SO. A case report of oculofacial rosacea complicating to corneal infiltrates and vascularisation. Trop J Ophthalmol Otolaryngol. 2020;5(2):60-62. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/133 |


 ©
©