Otogenic abscess: rarity and reality
Vishwanath Kale M.1*, C. Chhabria S.2, Sharma M.3, Subhash Gaikwad N.4
DOI: https://doi.org/10.17511/jooo.2020.i01.05
1* Meena Vishwanath Kale, Senior Resident, Department of ENT, T.N.M.C. & B.Y.L.Ch. Nair Hospital, Mumbai, Maharashtra, India.
2 Sanjay C. Chhabria, Assistant Professor, Department of ENT, T.N.M.C. & B.Y.L.Ch. Nair Hospital, Mumbai, Maharashtra, India.
3 Manisha Sharma, Junior Resident, Department of ENT, T.N.M.C. & B.Y.L.Ch. Nair Hospital, Mumbai, Maharashtra, India.
4 Ninad Subhash Gaikwad, Professor & HOD, Department of ENT, T.N.M.C. & B.Y.L.Ch. Nair Hospital, Mumbai, Maharashtra, India.
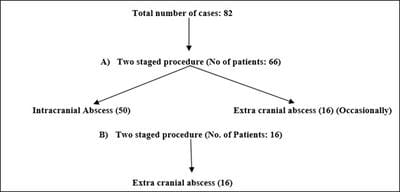
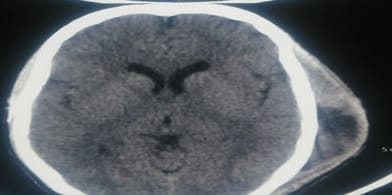
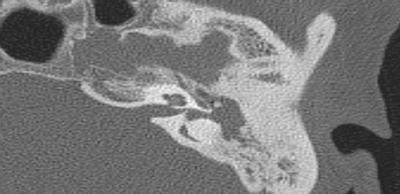
Introduction: Otogenic abscess is a complication commonly arising from active squamous chronic otitis media. It is rare (1:10000) but in fact are a dangerous reality to be managed promptly. Materials and Methods: A retrospective study of 82 cases of otogenic abscesses were studied over a period 24 years by simple random sampling. Cases of ear malignancy, previously operated mastoidectomy were excluded from study. All postop cases were analysed. Result: Most commonly affected were male (63.4%) in the second decade (34.1%) of life. Commonest bacterial infection was staphylococcus aureus (31.7%). Conclusion: Otogenic abscess though rare, are a reality and should be suspected when the patient with chronic ear discharge has high grade fever, severe headache and does not respond to best medical line of treatment. All these patients were subjected to imaging neurosurgical I&D of brain abscess followed by canal wall down tympano-mastoidectomy.
Keywords: Canal wall down tympano-mastoidectomy, Extracranial, Incision & Drainage (I &D), Intracranial, Otogenic abscess, Squamous active chronic otitis media
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Senior Resident, Department of ENT, T.N.M.C. & B.Y.L.Ch. Nair Hospital, Mumbai, Maharashtra, India. Email: |
Kale MV, Chhabria SC, Sharma M, Gaikwad NS. Otogenic abscess: rarity and reality. Trop J Ophthalmol Otolaryngol. 2020;5(1):22-29. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/127 |


 ©
©