Orbital cysticercosis: varied presentations with management plan
Sajid N.1, Sen P.2*
DOI: https://doi.org/10.17511/jooo.2020.i03.02
1 Noorjahan Sajid, Professor, Department of Ophthalmology, F.H. Medical College, Agra, Uttar Pradesh, India.
2* Priyangee Sen, Assistant Professor, Department of Ophthalmology, F.H. Medical College, Agra, Uttar Pradesh, India.
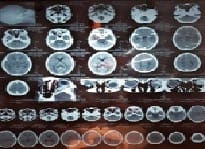
Introduction: Cysticercosis is a systemic parasitic disease caused by the larval form of the cestode pork tapeworm, Taenia solium. Along with subcutaneous tissue and skeletal muscles, eyes, brain, bladder wall, and heart are also the commonly involved sites of lodgment of the larva. The larval lodgment at these sites causes potentially harmful and variable clinical manifestations. Ocular cysticercosis can be extraocular or intraocular. Material and Methods: An immunologic reaction with fairly intense inflammatory signs and symptoms may be produced, and the surrounding structures may be compressed. Acquired strabismus, diplopia, recurrent redness, and painful proptosis are some of the clinical signs in patients with orbital cysticercosis. The present study report 8 cases of ocular cysticercosis with a variety of clinical presentations depending on the exact site of larval involvement. Result: Patient CT Scan was done to confirm the clinical diagnosis in most of the posterior segment and orbital lesions. Rest investigations were within normal limits. Conclusions: It becomes important to report these cases because of the relative rarity of the condition these days, myriads of presentation and age group, the relative concentration of cases in endemic areas, and CT Scan used as the definitive investigation to confirm orbital cysticercosis and rule out neurocysticercosis.
Keywords: Ocular cysticercosis, Myocysticercosis, Taenia solium, CT Scan
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Ophthalmology, F.H. Medical College, Agra, Uttar Pradesh, India. Email: |
Sajid N, Sen P. Orbital cysticercosis: varied presentations with management plan. Trop J Ophthalmol Otolaryngol. 2020;5(3):66-71. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/113 |


 ©
©