Study of ophthalmic manifestations in blood dyscrasias
Tyagi S.1*, Som V.2, Kumar K.3, Nigam R.4
DOI: https://doi.org/10.17511/jooo.2021.i05.01
1* Shreya Tyagi, Resident, Department of Ophthalmology, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
2 Vivek Som, Associate Professor, Department of Ophthalmology, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
3 Kavita Kumar, Head of The Department, Department of Ophthalmology, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
4 Rajendra Nigam, Professor, Department of Pathology, Gandhi Medical College, Bhopal, Madhya Pradesh, India.
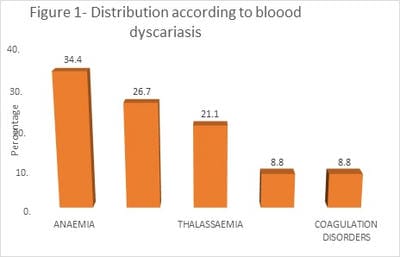
Background: We aimed to study the spectrum of ophthalmic manifestations in blood dyscrasias and assess the prevalence of ocular manifestations between acute and chronic blood malignancies. The study also aimed to correlate ophthalmic findings in anaemia, thalassaemia, leukaemia, lymphomas and other bleeding disorders. Methodology: The study was conducted as an observational study on a total of 180 patients diagnosed with blood dyscrasias at the Department of Ophthalmology, tertiary care hospital, during the study period of 2 years. Detailed history and examination were conducted, and findings were noted. All relevant haematological investigations were also done. Results: Out of 180 cases, anaemia was the most common diagnosis (34.4%). In patients with anaemia, 61.2% of subjects had normal findings, whereas 38.7% of cases had conjunctival pallor. However, in sickle cell anaemia, conjunctival pallor and comma sign was observed in 62.5% of patients each. Retinal Veinous Tortuosity was the most common finding in Thalassemia. In contrast, Veinous Fullness and Tortuosity and sub - conjunctival bleeding were the most common finding in patients with leukemia and coagulation disorders, respectively. Conclusion: Ophthalmic manifestations are commonly observed in patients with blood dyscrasia. The routine ocular examination must be conducted in cases of blood dyscrasias, and especially posterior segment evaluation should be mandatory in severe anaemia/ sickle cell haemo - globinopathy and leukaemia, which is both diagnostic and prognostic of the severity of this disease. Also, there is a need to develop a standard referral protocol between the haematology clinic and the eye clinic so that blood dyscrasia patients can have periodic evaluations.
Keywords: Opthmological manifestations, Blood dyscrasia, Anemia, ITP, Coagulation disorders
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Resident, Department of Ophthalmology, Gandhi Medical College, Bhopal, Madhya Pradesh, India. Email: |
Shreya Tyagi, Vivek Som, Kavita Kumar, Rajendra Nigam, Study of ophthalmic manifestations in blood dyscrasias. Trop J Ophthalmol Otolaryngol. 2021;6(5):85-92. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/210 |


 ©
©