Analysis of visual outcome of Neodymium: Yttrium-Aluminum -Garnet (Nd: YAG) laser capsulotomy in patients with Posterior Capsule Opacification
Deepa R.1*, A. Veeramani V.2
DOI: https://doi.org/10.17511/jooo.2020.i08.03
1* Deepa R., Junior Resident, Department of Ophthalmology, Saveetha Medical College, Chennai, Tamil Nadu, India.
2 V. Panimalar A. Veeramani, Assistant Professor, Department of Ophthalmology, Saveetha Medical College, Chennai, Tamil Nadu, India.
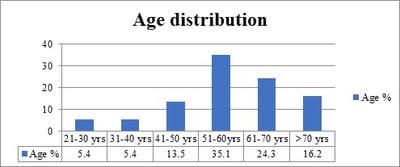
Objective: Posterior capsular opacification (PCO) is a postoperative complication causing decreased visual acuity. This study aims to study the efficacy of Nd: YAG laser capsulotomy in posterior capsular opacification following cataract surgery by analyzing the visual outcome. Material and Methods: A prospective study included a sample size of 50 eyes of 37 patients with Posterior capsular opacification following uneventful cataract surgery with significantly decreased visual acuity. Detailed anterior and posterior segment examination was done, best-corrected visual acuity (BCVA) was recorded along with measurement of IOP. Posterior capsulotomy was performed using Nd: YAG laser (Neodymium: Yttrium-aluminum–garnet) and patients were followed up. Visual acuity was assessed and complications if any were recorded. Results: It was noted that 74% of the patients at the end of 1st week and 78% of the patients at the end of 1st and 3rd month had significant visual improvement following Nd: YAG laser capsulotomy. There was a statistically significant difference in Post Nd: YAG laser BCVA on follow up with P-value <0.001. Complications encountered were the rise in IOP in 6% of the population at the end of 1 hour and 1st day of the procedure, iris bleeding was noted in 4% of the population, intraocular lens damage in 2 %, and cystoid macular edema in 2 % of the study population.
Keywords: Nd: YAG laser capsulotomy, Posterior capsular opacification
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Junior Resident, Department of Ophthalmology, Saveetha Medical College, Chennai, Tamil Nadu, India. Email: |
Deepa R, A Veeramani VP. Analysis of visual outcome of Neodymium: Yttrium-Aluminum -Garnet (Nd: YAG) laser capsulotomy in patients with Posterior Capsule Opacification. Trop J Ophthalmol Otolaryngol. 2020;5(8):216-223. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/175 |


 ©
©