A rare case report of Blepharophimosis syndrome associated with esotropia and nystagmus
Kalaria H.1*, Sabnis M.2, Kulkarni V.3, Devkar P.4
DOI: https://doi.org/10.17511/jooo.2020.i06.08
1* Hardik Kalaria, MBBS, 3rd Year Resident, Department of Ophthalmology, Dr. D. Y. Patil Medical College Hospital and Research Institute, Kolhapur, Maharashtra, India.
2 Milind Sabnis, Professor and Head, Department of Ophthalmology, Dr. D. Y. Patil Medical College Hospital and Research Institute, Kolhapur, Maharashtra, India.
3 Vedesh Kulkarni, MBBS, 3rd Year Resident, Department of Ophthalmology, Dr. D. Y. Patil Medical College Hospital and Research Institute, Kolhapur, Maharashtra, India.
4 Parag Devkar, MBBS, 2nd Year Resident, Department of Ophthalmology, Dr. D. Y. Patil Medical College Hospital and Research Institute, Kolhapur, Maharashtra, India.
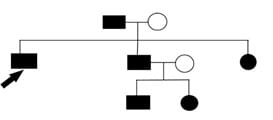
The authors report here a rare case of blepharophimosis syndrome which was associated with esotropia and nystagmus. Blepharophimosis syndrome is a clinical entity characterized by blepharophimosis, ptosis, epicanthus inversus, and telecanthus. In our case, it was also associated with horizontal nystagmus and esotropia. Our patient also had a bilateral mature cataract. It can either be type 1 or type 2 depending on the associated systemic manifestations. The present study describes a case of BPES type 2 with associated nystagmus and esotropia with a bilateral mature cataract.
Keywords: BPES syndrome, Blepharophimosis, Ptosis, Epicanthus inversus, Telecanthus, Nystagmus and esotropia
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , MBBS, 3rd Year Resident, Department of Ophthalmology, Dr. D. Y. Patil Medical College Hospital and Research Institute, Kolhapur, Maharashtra, India. Email: |
Kalaria H, Sabnis M, Kulkarni V, Devkar P. A rare case report of Blepharophimosis syndrome associated with esotropia and nystagmus. Trop J Ophthalmol Otolaryngol. 2020;5(6):163-167. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/156 |


 ©
©