A study of leave against medical advice (LAMA) in eye camp patients of ophthalmology department in a tertiary care center
Shivaji Navale A.1, Ramachandra S.2*, Rashmi G.3
DOI: https://doi.org/10.17511/jooo.2020.i06.03
1 Apurva Shivaji Navale, 3rd Year Post-Graduate, Department of Ophthalmology, Sri Devaraj Urs Medical College, Kolar, Karnataka, India.
2* Sandhya Ramachandra, Professor and Head of Department, Department of Ophthalmology, Sri Devaraj Urs Medical College, Kolar, Karnataka, India.
3 Rashmi G., Assistant Professor, Department of Ophthalmology, Sri Devaraj Urs Medical College, Kolar, Karnataka, India.
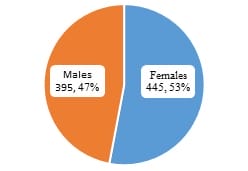
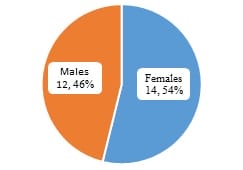
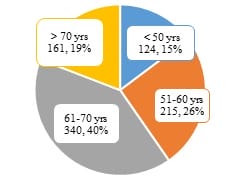
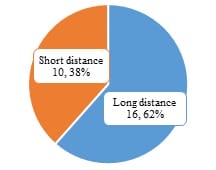
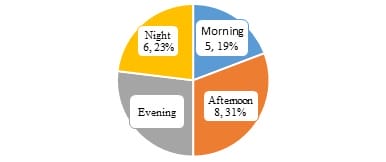
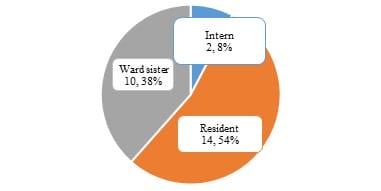
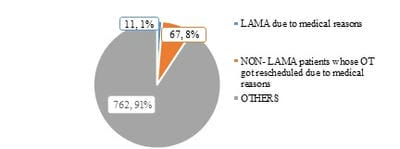
Introduction: To scientifically document and understand Leave Against Medical Advice (LAMA) characteristics of the patients selected for comprehensive eye care management from rural eye campsite. Methods: This was a cross-sectional study, where the demographic details, diagnosis, and details of LAMA were documented and then analyzed to find out if any peculiar pattern was seen among them. Results: Out of 840 patients over a period of 7 months, 26 (3.09 %) were seen leaving against medical advice, the majority being females (54 %). Most of the patients were in the age group of 61-70 years (42.3 %) and from long-distance camps (61.5%). They were accompanied by one of the family members (42.2%), with the majority of them leaving due to medical reasons (43.3%), seen mostly in the rainy season and festive months. Conclusion: LAMA is an indicator of the effectiveness of the community health care delivery system. Better insight into the reason requires understanding their social, economic, cultural, and educational status. Reducing the number of LAMA patients can have a positive impact on the optimal utilization of resources and improve the health status of the community.
Keywords: LAMA, leave against medical advice, Ophthalmology, Outpatient department, Cataract, Eye camp
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor and Head of Department, Department of Ophthalmology, Sri Devaraj Urs Medical College, Kolar, Karnataka, India. Email: |
Navale AS, Ramachandra S, Rashmi G. A study of leave against medical advice (LAMA) in eye camp patients of ophthalmology department in a tertiary care center. Trop J Ophthalmol Otolaryngol. 2020;5(6):131-137. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/152 |


 ©
©