Prognostic factors in Pars Plana vitrectomy for Proliferative Diabetic Retinopathy
Rukmangathan K.1*, P. N.2, Ravichandran R.3, Chandrasekaran R.4
DOI: https://doi.org/10.17511/jooo.2020.i06.01
1* Keerthivarman Rukmangathan, Associate Professor, Department of Ophthalmology, Annapoorana Medical College, Salem, Tamil Nadu, India.
2 Nandhakishore P., Consultant, Aravind Eye Hospital, Theni, Tamil Nadu, India.
3 Ramusiddharthan Ravichandran, Consultant, Sri Ramanamaharishi Eye Hospital, Thiruvannamalai, Tamil Nadu, India.
4 Ranjan Chandrasekaran, Consultant, Annai Eye Hospital, Ramanathapuram, Tamil Nadu, India.
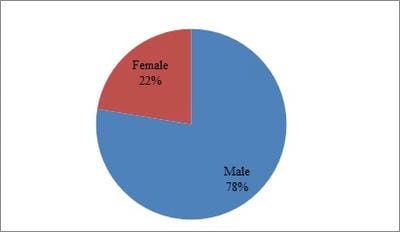
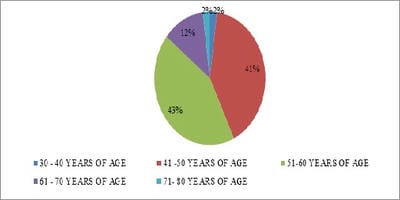
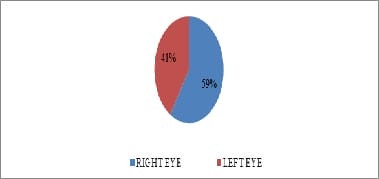
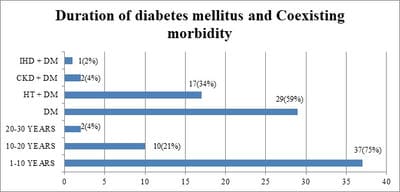
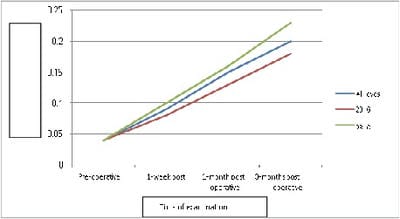
Objective: To determine the factors associated with good visual outcome in eyes undergoing pars plana vitrectomy (PPV) for proliferative diabetic retinopathy (PDR). Furthermore, the objective of the study was to compare the clinical outcome and complications of standard 20 gauge vitrectomy with 23-gauge transconjunctival sutureless vitrectomy. Materials and Methods: This was a prospective interventional study performed on patients presenting at the Retina clinic of a tertiary eye care hospital in Salem, Tamil Nadu between October 2018 to November 2019. All eyes undergoing PPV for complications of PDR and having adequate follow were included. The patients were divided into two groups, one group undergoing standard 20 gauge vitrectomy and the other group undergoing 23 gauge transconjunctival sutureless vitrectomy. Results: A total of Forty-nine eyes (25 eyes underwent standard 20 gauge vitrectomy and 24 eyes underwent 23 gauge transconjunctival sutureless vitrectomy). Visual acuity improved significantly following PPV (p<0.0001) and this improvement was seen in both 20 gauge group (p=0.0004) and in 23 gauge group (p=0.00005). There was no significant difference in best-corrected visual acuity noted between the two groups. However, eyes that underwent 23 gauge vitrectomy tended to gain vision earlier when compared to eyes that underwent 20 gauge vitrectomy. Complications following vitrectomy did not differ significantly between 20 gauge and 23 gauge group. Conclusion: Visual acuity improved significantly following PPV across all indications. Visual acuity in eyes that underwent 23 gauge TSV tended to gain vision earlier than eyes that underwent standard 20 gauge vitrectomy.
Keywords: Proliferative diabetic retinopathy, Pars plana vitrectomy, Non-proliferative diabetic retinopathy
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Ophthalmology, Annapoorana Medical College, Salem, Tamil Nadu, India. Email: |
Rukmangathan K, Nandhakishore P, Ramusiddharthan R, Chandrasekaran R. Prognostic factors in Pars Plana vitrectomy for Proliferative Diabetic Retinopathy. Trop J Ophthalmol Otolaryngol. 2020;5(6):116-124. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/148 |


 ©
©