Schwannoma of the submandibular gland: A rare case report
Ravinder Raja K.1*, Basha Shaik F.2
DOI: https://doi.org/10.17511/jooo.2020.i04.03
1* Khetawat Ravinder Raja, Assistant Professor, ENT Department, Mahavir Institute of Medical Sciences, Vikarabad, Telangana, India.
2 Feroz Basha Shaik, Assistant Professor, ENT Department, Mahavir Institute of Medical Sciences, Vikarabad, Telangana, India.
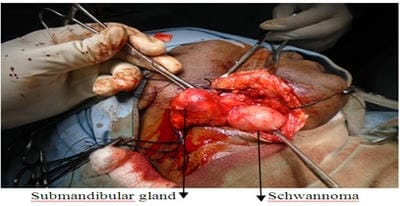
Schwannoma is a slow-growing, benign, encapsulated tumour of Schwann cells, which form myelin in peripheral nerve. It is the most common tumour of peripheral nerve, also known as neurilemma or neurinoma. Schwannomas of head and neck area are common and may arise from peripheral, central or autonomic nerve but salivary gland schwannomas are rare extracranial forms. The present study reports a rare case of schwannoma of the submandibular gland in a 42-year-old male patient which is presented with a painless mass in the submandibular region, treated by total excision of the submandibular gland. There were postoperative nerve deficit and no recurrence within 3months of follow up.
Keywords: Neurilemoma/Neurimoma, Tumour, Schwannomas, Submandibular gland
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, ENT Department, Mahavir Institute of Medical Sciences, Vikarabad, Telangana, India. Email: |
Raja KR, Shaik FB. Schwannoma of the submandibular gland: A rare case report. Trop J Ophthalmol Otolaryngol. 2020;5(4):96-99. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/139 |


 ©
©