Bilateral optic disc edema: causes and clinical features at a tertiary center in South India
Ijeri R.1*, Jyoti RC.2
DOI: https://doi.org/10.17511/jooo.2020.i02.03
1* Raghavendra Ijeri, Assistant Professor, Department of Ophthalmology, Sri B M Patil Medical College Hospital and Research Centre, Vijayapur, Karnataka, India.
2 Jyoti RC, Senior Resident, Department of Ophthalmology, Sri B M Patil Medical College Hospital and Research Centre, Vijayapur, Karnataka, India.
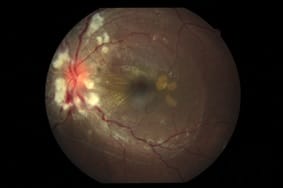
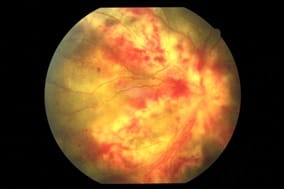
Aims: Bilateral optic disc edema: causes and clinical features at a tertiary center in South India. Bilateral Optic disc edema is one of the important fundus findings. Many times it indicates systemic pathology. The current study evaluated various causes of bilateral optic disc edema. Settings and Design: Prospective study. Methods and Material: This prospective study was conducted at a tertiary hospital in north Karnataka part of India (southern India). This study was conducted from June 2016 to November 2018. Detailed ocular examination including vision, slit-lamp examination, Visual field analysis, detailed fundus evaluation using an indirect ophthalmoscope, 78 Dioptre lens and fundus camera was done. Systemic investigations like blood examination and radiological investigations like Computerized tomography (C.T), Magnetic Resonance Imaging (MRI) were done whenever required. Results: A total of sixty-three cases with bilateral optic disc edema was recorded in this study. Thirty were females and thirty-three were males. Out of these, 36 cases had papilledema (increased intracranial pressure), 7 cases had optic neuritis, 6 cases of hypertensive retinopathy, 5 patients had Vogt Koyanagi Harada Syndrome (VKH), 3 had neuroretinitis, Cytomegalovirus (CMV) retinitis in 2 cases and in 4 cases causes could not be found. Total of 36 (57.14%) patients had papilledema, 7 (11.11%) had optic neuritis, 3 (4.8%) patient had neuroretinitis, 6 (9.52%) cases of hypertensive retinopathy, 5 (7.9%) patient had VKH, CMV retinitis in 2 (3.2%) and 4 (6.3%) idiopathic. Conclusions: Papilledema was the commonest cause followed by optic neuritis for bilateral optic disc edema.
Keywords: Bilateral Optic disc edema, Papilledema, Optic Neuritis, South India
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Ophthalmology, Sri B M Patil Medical College Hospital and Research Centre, Vijayapur, Karnataka, India. Email: |
Ijeri R, Jyoti RC. Bilateral optic disc edema: causes and clinical features at a tertiary center in South India. Trop J Ophthalmol Otolaryngol. 2020;5(2):55-59. Available From https://opthalmology.medresearch.in/index.php/jooo/article/view/124 |


 ©
©